Fig. 4—Uterine arteriovenous malformation (AVM) in two different
patients.
A and
B, 36-year-old
woman who presented with persistent hemorrhage after dilation and curettage for
retained products of conception (RPOC). Transverse images from transvaginal
ultrasound (A)
show echogenic material within uterine cavity, with increased flow on color
Doppler sonography (B).
Spectral Doppler sonography shows low resistance waveform and peak systolic
velocity of approximately 60 cm/s (not shown). Possibility of AVM was raised.
Pathologic examination after hysterectomy revealed adherent RPOC and no AVM.
C–F, 22-year-old woman who presented with intermittent heavy
vaginal bleeding 6 weeks after elective first trimester termination.
Physiologic bleeding was noted in first month after procedure, which
accelerated 2 weeks before presentation. Serum β-HCG was
nondetectable. Transvaginal ultrasound (C) shows clot within endometrial cavity with eccentric vascular
mass in fundus. Waveform on spectral Doppler sonography was low resistance,
with peak systolic velocity greater than 90 cm/s (not shown). Vascular
malformation was suspected, and patient was referred for angiography. Multiple
images from pelvic angiogram show prominent right uterine arteries (arrow, D).
Subsequently, there is vascular blush of presumed AVM in fundus (arrow, E)
and then early filling of draining vein (arrow, F).
This was embolized with cessation of patient bleeding. No pathologic analysis
was available to confirm vascular malformation. Although history and
angiographic features were suggestive of AVM, chronic RPOC can simulate
ultrasound and angiographic appearance of AVM and cannot be excluded as reason
for bleeding in this case.



The postpartum period is defined as beginning immediately after the delivery
of the infant and placenta and typically is considered to continue for 6–8
weeks as the physiologic changes of pregnancy slowly revert to baseline. The
period after a spontaneous or elective abortion is less well defined, but
complications are often grouped into early complications occurring immediately or within the first days
after the procedure and delayed complications occurring beyond that time [1,
2].
Pregnancy remains a major cause of
mortality in the 21st century in the United States. A recent analysis placed
the pregnancy-related mortality rate at 14.5 deaths/100,000 live births, with
more than three quarters of deaths occurring in the postpartum period (most
commonly related to hemorrhagic or embolic conditions) [3]. In addition to
these life-threatening complications, other conditions such as endometritis and
retained products of conception (RPOC) are relatively common after birth or
termination and may require hospitalization or additional procedures [4, 5].
Finally, almost one third of births in the United States are now performed by
cesarean section, which results in the possibility for both immediate and
delayed complications [6]. Because of their prevalence, a radiologist must be
familiar with the various postpartum complications and the role imaging plays
in their clinical evaluation.
Imaging the Postpartum Uterus
The postpartum uterus typically
requires 6–8 weeks to involute and return to its typical nongravid size and
appearance on ultrasound [7]. Although ultrasound is often performed in this
period to evaluate for abnormalities such as RPOC, imaging of the postpartum
uterus is complicated: the postpartum uterus has a variable appearance, and
there is significant overlap between the normal and abnormal uterus (Fig. 1).
For example, echogenic material is frequently seen within the uterus in
patients with bleeding, but this was found in one study not to be predictive of
need for further intervention [8]. In a prospective study of asymptomatic women
with physiologic levels of vaginal bleeding after delivery, an echogenic
endometrial mass was present in half of the patients 7 days postpartum and in
21% of subjects at 2 weeks [9]. The entire postpartum uterus can appear
hypervascular on color Doppler images, which will typically spontaneously
resolve without incident [10]. The presence of gas within the endometrial cavity,
either on CT or as echogenic shadowing foci on ultrasound, may also be a normal
finding for several weeks after delivery [10, 11].
RPOC and Postpartum Hemorrhage
RPOC is a nonspecific term that
encompasses residual fetal or placental tissue remaining after delivery,
miscarriage, or termination.
The frequency of RPOC has been variably
described. It most commonly occurs with spontaneous abortions, with a frequency of up to 22% [4]. However, RPOC are
quite uncommon after elective termination [12]. Primary postpartum hemorrhage
is defined as blood loss greater than 500 mL after vaginal birth and greater
than 1000 mL after cesarean section. The most ommon cause is an atonic uterus,
which does not contract to halt hemorrhage. Atony can result from numerous causes,
such as extended labor, multiple gestations or a large fetus, or use of
oxytocin for induction or augmentation. Incomplete delivery of the placenta is
an important cause of uterine atony and is often suspected when the placenta
fails to deliver, delivers incompletely, or has evidence of fragmentation.
Secondary postpartum hemorrhage occurs
when bleeding begins more than 24 hours after delivery; it is less common than primary
hemorrhage but can cause significant morbidity and mortality [13]. RPOC is an
important cause of secondary hemorrhage, and ultrasound is often requested for
evaluation, whereas RPOC causing primary hemorrhage are often suspected and
treated at the time of delivery without imaging.
Placenta accreta is a spectrum of
conditions involving a placenta that is abnormally adherent to the endometrium
and is an important cause of RPOC and postpartum hemorrhage [14]. Placenta
accreta vera occurs when the chorionic villi contact but do not invade the
myometrium, placenta increta occurs when there is myometrial invasion, and placenta
percreta involves invasion to or through the uterine serosa. Placenta accreta
typically develops where there is a deficiency of the decidua basalis (e.g.,
cesarean scar) and is particularly likely in patients with placental previa or
multiple cesarean sections. However, it can also occur after termination and
prior uterine procedures and with advanced maternal age, uterine anomalies,
Asherman syndrome, or subserosal fibroids [15]. The
imaging of placenta accreta will be discussed in greater detail later in this
article (see the Delayed Cesarean Complications subsection).
Ultrasound Appearance of RPOC
Although it can be also be a normal
postpartum finding, the presence of an echogenic mass in the endometrium
appears to be the most accurate sign of RPOC, as
determined by a retrospective review of 163 patients with suspicion for RPOC
that reported sensitivity and specificity of 79% and
89%, respectively [16]. Increased color Doppler flow, which can also be
physiologic in the postpartum period, was found in the same study to be more
prevalent with RPOC than without it (79% vs 40%) (Figs. 2 and 3). Another cohort
study of 265 women found that the presence of an intrauterine mass on routine postpartum
ultrasound in asymptomatic women with uneventful deliveries was found to be
predictive of future hemorrhage and the need for surgical intervention [17].
However, a smaller study did not show this result [8]. The significance of
apparent endometrial stripe thickening, typically greater than 10 or 13 mm, has
been reported in one study to be a useful indicator of RPOC [18], whereas multiple others have not [8, 17, 19,
20].
The most important message regarding RPOC
is that no single factor has perfect positive or negative predictive values.
Because both clinical signs and symptoms and ultrasound findings have high
false-positive rates, being conservative in diagnosing RPOC and not relying on
a single indicator are important principles that should guide reporting [21].
Uncommon Causes of Hemorrhage
Subinvolution of the placental site is
a likely underrecognized cause of postpartum hemorrhage because it can be
diagnosed only by pathologic analysis after
hysterectomy or sufficient uterine curettage. In this condition, even in the
absence of a cause such as RPOC, the uteroplacental
arteries fail to regress and result in significant bleeding. There may be an
immunologic basis for this condition through a common mediator that causes
these vessels to regress prematurely in eclampsia [22]. This condition has no
characteristic imaging findings.
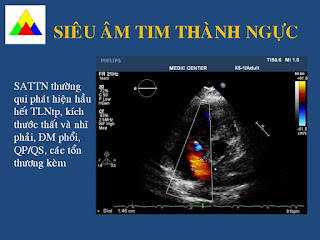
Uterine arteriovenous malformations (AVMs)
are an exceedingly rare cause of postpartum bleeding. They can be congenital or acquired as a result of hormonal
stimulation, but the most common cause is likely iatrogenic. A mass in the
postpartum uterus
with vascularity on ultrasound is much
more likely to represent RPOC than AVM. AVM can be considered when RPOC have
been excluded and the mass is hypoechoic on B mode images and located within
the myometrium [23] (Fig. 4). The presence of low-resistance waveforms and peak
velocities greater than 80 cm/s have been described as features suggestive of
AVM over other causes [24].
Some authors think that uterine
vascular malformations have been overdiagnosed recently because hypervascular
masses that simulate the appearance of a true
vascular malformation can develop around RPOC in the endometrial cavity or
myometrium.
The possibility of a vascular
malformation in postpartum patients may delay curettage for fear of provoking
hemorrhage, despite a lack of definitive evidence to suggest this as a
complication [25]. Conservative therapy and observation have been suggested for
stable patients with a suspected vascular malformation, and embolization or
hysterectomy is recommended only for unstable patients.
A traumatic pseudoaneurysm may appear and
behave similarly but is likewise quite rare. Turbulent bidirectional flow
within the
pseudoaneurysm may resemble the Chinese-Taoist
yin and yang symbol (yin-yang sign) on color Doppler images, as pseudoaneurysms
do elsewhere in the body [26].
Interventional Radiology and
Postpartum Hemorrhage
In cases of life-threatening
postpartum hemorrhage that does not respond to uterine massage and medical
therapy, the traditional
method of treatment has been
hysterectomy. Although definitive, it is an invasive procedure that sacrifices
future fertility. Uterine artery embolization is an alternative method for
treatment of postpartum hemorrhage [27].
Embolization has been used to treat
uterine atony resulting from multiple causes. Embolization is the therapy of
choice for rare vascular causes of postpartum hemorrhage, such as uterine
pseudoaneurysms and vascular malformations. Embolization as well as balloon occlusion
of the iliac arteries has also been used in prophylaxis and treatment of placenta
accreta. Embolization has been reported to be efficacious in small case series,
especially when performed as a prophylactic measure when the diagnosis is known
[28, 29]. The role of balloon occlusion of the iliac arteries is more
controversial, with varying efficacy reported in the literature [30, 31].
The rate of successful treatment with
embolization is high (near 90%) and appears to have a negligible effect on
future fertility [25]. Often, uterine artery
embolization can successfully control hemorrhage even if there is no evidence
of active extravasation
(Fig. 5). Because uterine fibroid
embolization has emerged as a modality for treatment of symptomatic uterine
leiomyoma, interventional radiologists are likely to be increasingly comfortable
utilizing similar techniques for the control of postpartum hemorrhage.
Endometritis and Postpartum Infection
Endometritis, or infection of the
uterine decidua, is the most common cause of postpartum fever. Although a
low-grade fever is expected in the first 24 hours
after vaginal delivery or cesarean section, fever after this period is
suspicious for endometrial infection.
Endometritis is more common after cesarean
section, with rates up to 30 times higher than that after spontaneous vaginal delivery [32]. The rates are higher
when prophylactic antibiotics are not used, such as for emergent cesarean
sections or some cases of therapeutic abortions [6, 33].
Endometritis is a clinical diagnosis,
but uterine imaging is sometimes requested to guide therapeutic decisions.
Typically, endometritis is treated with broad spectrum antibiotics, but if
RPOC, infected hematoma, or uterine abscess are present, evacuation may be
required.
Not surprisingly, the evaluation of
endometritis is fraught with the same issues as for other postpartum imaging,
with considerable overlap between physiologic and abnormal findings. Patients
with clinical endometritis can have normal ultrasound findings, echogenic material
within the uterus can be normal in postpartum women and may not reflect
infected hematoma or RPOC, and endometrial gas can be a normal finding for up
to 3 weeks after delivery and does not always indicate infection [34] (Fig. 6). Again, not being overly
reliant on or definitive according to a single finding and integrating the
imaging findings into the complete clinical picture is
crucial.
One potential but rare complication of
endometrial infection is pelvic septic thrombophlebitis. This occurs in
approximately one in 2000 deliveries and 1–2% of cases of endometritis; it
appears to be more prevalent when the infection spreads to the parametrial
tissues [32]. CT or MRI is preferred over ultrasound in the evaluation of
patients for whom conventional antibiotic therapy has failed and who are
suspected of having underlying conditions, such as septic thrombophlebitis or an
abscess. Both modalities will typically show an expanded ovarian vein with
internal thrombus (Fig. 7). Enhancement of the vessel wall may also be present.
Treatment is anticoagulation in addition to antibiotic therapy.
Thrombotic Complications
Pregnancy has long been recognized as
a prothrombotic state. The mechanism of this thrombophilia is thought to be due
to increased levels of fibrin and the other coagulation factors, as well as
systemic up-regulation of plasma prothrombotic mediators.
This synergizes with the slowed lower
extremity venous velocities that develop in the third trimester to predispose
patients to deep vein thrombosis and pulmonary embolism [35]. Complications of
venous thromboembolism are the leading cause of mortality of pregnant and
recently pregnant women within the developed world [36].
Like other changes of pregnancy, the
prothrombotic state of pregnancy does not immediately revert to normal after
delivery.
The rate of pulmonary embolism has
been found to be highest in the postpartum period, and it requires 4 weeks for
the risk of venous thromboembolism to return to normal population levels after
delivery [37].
The evaluation of pregnant and
postpartum women with suspected pulmonary embolism has been extensively
discussed and
remains a controversial topic [38,
39]. In the postpartum period, concerns about fetal exposure to ionizing
radiation or gadolinium is no longer a factor. However, ionizing radiation exposure
to actively dividing and lactating breast tissue remains an important issue.
Many practicing radiologists continue
to recommend CT angiography because of its high sensitivity and specificity and
its ability to evaluate for other causes of dyspnea or chest pain [38, 40].
However, ventilation perfusion or perfusion-only scintigraphy has advantages,
including a lower dose to breast tissue [41, 42]. In addition, in pregnant
patients, there is a reported higher rate of nondiagnostic CT angiograms
potentially due to alterations in maternal cardiac output [43]; this could
extend into the postpartum period as well. Because of this continued debate, provider
and patient preference will likely decide which test is favored in an
institution.
Additional thrombotic complications in
pregnancy include ovarian vein thrombosis and thrombophlebitis, as mentioned
previously in this article. Thrombosis of a dural sinus or cerebral vein is a
rare but important cause of postpartum headache, altered mental status,
seizure, and other neurologic symptoms and occurs more frequently in the
postpartum period than during pregnancy [44].
These patients tend to have better
outcomes when treated, compared with other patient groups with venous sinus
thrombosis. CT or MR venography should be considered for the evaluation of new
neurologic symptoms in the postpartum period. The sensitivity of unenhanced head
CT for the detection of venous sinus thrombosis is relatively low (25–64%).
Venous sinus thrombosis should be
suspected as a potential underlying cause of brain parenchymal abnormalities
(e.g., edema or hemorrhage) in the postpartum period [45] (Fig. 8).
Finally, amniotic fluid embolism is a
rare but feared complication of labor. Because of trauma to the ovarian veins
during labor, amniotic fluid is able to enter the venous circulation [46]. The
classic clinical presentation is rapid onset of shock and respiratory collapse.
Chest radiographs will typically show new
bilateral pulmonary opacities that appear similar to acute pulmonary edema.
Cesarean Delivery and Other Surgical Complications
Immediate or Early Complications
As discussed earlier, the rate of
cesarean delivery has increased substantially in the past two decades and is
now the most commonly performed surgical procedure in U.S. hospitals [6]. The
potential reasons for this increase include changing patient demographics (such
as increased frequency of multiple births), but it is more likely a reflection of
changes in patient and physician preference and medicolegal concerns.
Cesarean section has a much higher
rate of endometritis compared with vaginal delivery, and endometritis is the
most common complication after cesarean section
[47]. The risks common to any surgical procedure are also present after
cesarean section, such as significant bleeding and hematoma or wound infection.
Wound infection has been estimated to occur in about 5% of cases, most of which
will be diagnosed and treated clinically without requiring imaging [48].
When endometritis is diagnosed, either
clinically or with the aid of imaging, the typical treatment is antibiotics.
The majority of women will do well on this treatment,
although a low percentage of cases (8–10%) will be complicated by pelvic
abscess or thrombophlebitis [32, 49]. A rare but feared complication of
endometrial infection is uterine rupture due to infection and necrosis. Analogous
to infectious dehiscence of a fascial incision or surgical anastomosis, the
myometrial incision can become infected and dehisce, resulting in uterine
rupture. This condition is rare, with an estimated incidence of one in every 700–2400
cesarean births [50]. Uterine dehiscence may be suspected if the discontinuity is
felt on bimanual examination. For this condition, MRI appears to have superior
accuracy over CT, which may not be able to differentiate phlegmon or abscess in the region of the scar from true
dehiscence [51]. Findings that have been described on MRI include a lack of
apposition of the endometrium and serosa at the incision site and discontinuity
of the myometrium with associated fluid collection, hematoma, or regions of low
signal intensity suggestive of gas. Conservative management in cases of partial
dehiscence has been proposed with some success, but most patients undergo
hysterectomy.
Although smaller bladder wall
hematomas have been seen in normal cesarean section, the presence of large
hematomas (> 5 cm) has been associated with infective uterine rupture. Although
detection of uterine discontinuity has been described on ultrasound, its sensitivity
compared with that of MRI or CT has not been established in the literature.
Intraoperative complications of
cesarean section are not rare, especially when the indication is emergent; one
study found a 12.1% rate of intraoperative
complications. The majority of these complications are blood loss and
inadvertent injury to the uterus, along with cervical
lacerations; injury to the bladder, ureter, and bowel are more rare (≤ 1%) [52]. Patients who require
peripartum hysterectomy (i.e., hysterectomy performed immediately after a
delivery or as part of a surgical delivery) need special attention.
Peripartum hysterectomy can be either planned,
as in the case of suspected abnormal placentation, or emergent, because of bleeding complications. Peripartum
hysterectomy is associated with much higher rates of intraoperative bleeding,
urinary tract injuries, infections, and the need for additional operation or
procedures [53, 54] (Fig. 9).
When imaging is requested to evaluate for
postcesarean or other surgical complications, the standard contrast-enhanced CT
of the abdomen and pelvis acquired in
venous phase is often sufficient if the clinical concern is infection. If
significant abdominal ascites is known or identified on the examination, obtaining
a series in the excretory phase or performing a CT cystogram should be considered
to evaluate for ureteral or bladder injury. If uterine dehiscence is suspected either
clinically or on prior CT, contrast-enhanced pelvic MRI appears to be the
superior diagnostic modality.
Delayed Cesarean Complications
In addition to the complications
already discussed, there are complications of cesarean section that may not
become apparent until weeks or months after delivery or until future pregnancies.
These complications are primarily related to the uterine scar. Although
longterm complications secondary to bowel or urinary tract injury are possible,
they are rare.
Endometriosis at Cesarean Section
Scar
Endometriosis can develop in the
abdominal incision site after cesarean section (also known as a scar
endometrioma). Scar endometriosis is a rare complication with a reported incidence
ranging from 0.03% to 1.5% [55]. However, it is still the most common manifestation
of extragenital endometriosis [56]. This condition can have a variety of
clinical presentations. Pain can be constant or cyclically related to the
menstrual cycle. A palpable mass may or may not be present. Patients will often
not have a history of preexisting
endometriosis, and delays in diagnosis are not rare.
On ultrasound, scar endometriomas can have
a varied appearance based on size [55]. Small-to-moderate endometriomas in the abdominal wall are solid masses that
have less-well-defined borders and are less homogeneously hypoechoic than
pelvic endometriomas.
As they become larger (> 3 cm), more
cystic regions and even less-well-defined borders have been described. Flow may
be present on Doppler images in endometriomas of any size.
Postcesarean Placenta Accreta
The frequency of placenta accreta has been
increasing in the last decades likely as a result of increased utilization of
cesarean section. Accreta now affects one in
500 pregnancies; there is a high association with placenta previa as well [57].
Making the diagnosis of placenta accreta before the delivery is crucial because
it has been shown to reduce maternal morbidity [58, 59].
At the time of the fetal anatomy scan
(18–20 weeks), dedicated evaluation of the placenta and lower uterine segment
is suggested for any patient with a history of repeated cesarean sections or
with placenta previa. The sensitivity of ultrasound for the detection of accreta
has been reported to be as high as 90% [58] and as low as 30% in a small study of
13 patients [60]. Several ultrasound features have been identified to suggest
placenta accreta. The most sensitive sign is the presence of multiple placental
lacunae [61]. The pathophysiology of lacunae are unknown, but they appear as
hypoechoic foci that represent abnormal clusters of vessels with less
well-defined borders than normal venous lakes and often will show turbulent flow
on color Doppler images. They have been described as giving the placenta a “Swiss
cheese” or “moth-eaten” appearance. Several additional signs have been described
that include loss of the retroplacental clear space, gap in the retroplacental
blood flow, thinning and distortion of the myometrium, irregularity of the
bladder-uterine interface, and bulging of the placenta into the urinary
bladder.
If placenta accreta is convincing on
ultrasound, many clinicians will proceed with cesarean section and potential
hysterectomy.
If the finding is unclear, MRI of the pelvis
has been suggested as an alternative modality. The value of MRI has been
variably reported: studies have shown superior sensitivity
and specificity [62] and equivalent sensitivity and specificity to ultrasound, which may be helpful in indeterminate
cases [63], but another study failed to show that the information obtained by
MRI changed clinical management or outcomes [64]. The most well-described MRI
findings for placental invasion are bulging of the placenta that distorts the
normal uterine contour, the presence of dark intraplacental bands on T2-weighted
images, and a heterogeneous appearance of the placenta [65] (Fig. 10).
Cesarean Scar Implantation or
Ectopic Pregnancy
A pregnancy that develops within a
prior cesarean section scar has previously been considered one of the rarest
forms of abnormal implantation [66]. It has been suggested that these are not
ectopic pregnancies because they can, in rare circumstances, be carried to
term; however, these are considered as ectopic pregnancies for the purpose of
this discussion because there is implantation outside of the normal decidua and
a high rate of complications.
Although rare, the incidence of
cesarean scar implantation appears to be increasing. Again, this is likely
because of the increasing rate of cesarean delivery and increased recognition
[67]. On ultrasound, care must be taken to definitively identify the
gestational sac within the low transverse incision and not in the adjacent
adnexa, which cansimulate this condition (Fig. 11). Recognition of ectopic pregnancy within the uterus
itself is crucial because of the risk of uterine rupture and catastrophic
bleeding.
Although the rate of cesarean scar ectopic
pregnancy appears to be increasing, definitive guidelines for management have
yet to be outlined. A variety of treatment options have been used, ranging from
observation, medical treatment either systemic or locally injected, local
resection utilizing hysteroscopy or laparoscopy, laparotomy either for local
resection of the gestational sac or total hysterectomy, treatment with uterine
artery embolization, to a combination of these approaches.
Conclusion
The significant overlap between the
pathologic and physiologic changes of the postpartum uterus presents many
difficulties to interpreting ultrasound examinations in the postpartum period.
In addition, increasing rates of delivery by cesarean section have the possibility
to increase the frequency of early and late complications. It is crucial for
radiologists to be aware of the most common postpartum complications on which
they will be asked to consult and the strengths and limitations of the various
imaging modalities, so that they could assist in the appropriate care of these
patients.