By Theresa Pablos, AuntMinnie staff writer
September 3, 2020 -- Ultrasound may be the ideal imaging modality for evaluating palpable breast masses in lactating women, according to the results of a September 1 study in Radiology. For breastfeeding patients, targeted ultrasound identified just as many cancers as mammography with fewer false-positive findings.
The results are especially notable since more women in the U.S. are delaying childbearing into their 30s and 40s -- ages when mammography is typically considered the ideal first-line imaging modality for symptomatic patients. The findings support guidelines recommending the use of ultrasound for breastfeeding women of all ages.
"These findings suggest that sensitivity of mammography is slightly limited and inferior to that of [ultrasound] during pregnancy and lactation because of increased breast density," wrote the authors, led by Dr. Maggie Chung from the department of radiology and biomedical imaging at the University of California, San Francisco.
Ultrasound is often recommended as a first-line imaging modality for symptomatic, lactating women, but the evidence to support this recommendation for patients ages 30 and older is "near nonexistent," the authors noted. This lack of evidence prompted the team to conduct their own investigation.
The retrospective study included 167 lactating women with palpable breast masses who underwent ultrasound diagnostic evaluation at an academic institution between January 2000 and July 2017. The women were not currently pregnant and had no known malignancies at the time of evaluation. Their ages ranged from 17 to 52, with a median age of 35.
While all 167 women underwent ultrasound evaluation, 59% also underwent mammography. Mammography was performed at the discretion of the interpreting radiologist because the institution did not have a specific imaging policy for breastfeeding women -- a reflection of larger uncertainty around ideal imaging modalities for mothers in their 30s and 40s.
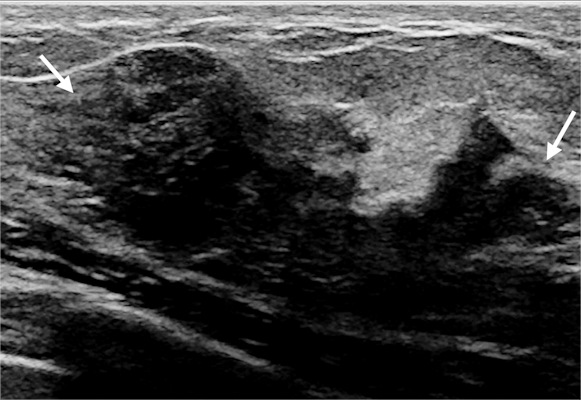
Targeted ultrasound scans identified a sonographic correlate to the palpable lump for 66% of women. A little more than half of these women had findings categorized as benign or probably benign, with cysts, inflammation or infectious changes, and galactoceles representing the most common benign findings.
An additional 53 women were recommended for biopsy due to a BI-RADS 4 or 5 lesion on the targeted ultrasound scan. Of these women, five were diagnosed with invasive ductal carcinoma. Mammography identified seven additional suspicious lesions but no additional cancers.
On its own, targeted ultrasound achieved a 100% sensitivity and 67% specificity. When combined with mammography, the modality maintained a 100% sensitivity rate, but the specificity rate dropped to 61%.
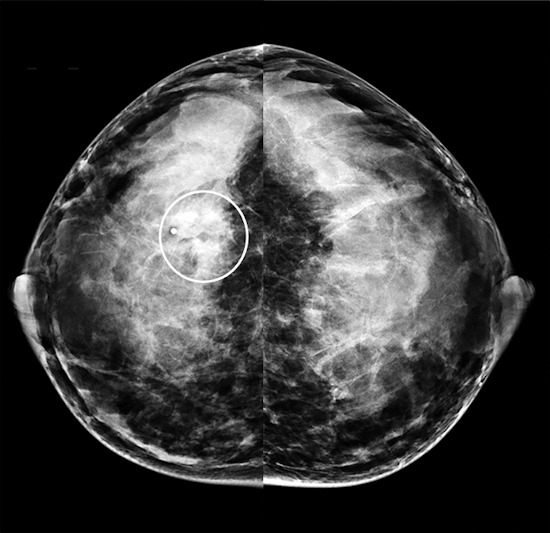
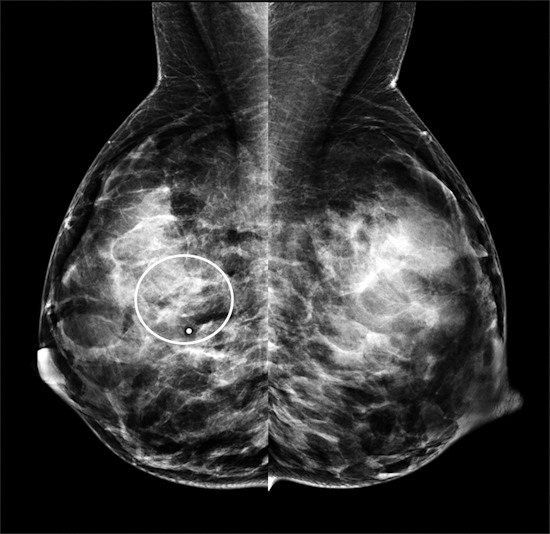
The authors attributed mammography's lower specificity due to the modality's struggle depicting cancers in dense breast tissues during pregnancy and lactation. Notably, 98% of the patients in the study had dense breast tissue, including 72% of whom had extremely dense breast tissue.
The authors cautioned that selection bias could have even overstated the performance of mammography in their study. Still, they noted mammography may benefit lactating women ages 40 or older, which only comprised a small subset of their study population.
"Mammography may be of greater benefit in lactating women age 40 years or older in whom the incidence of breast cancer is higher," they wrote. "More data are needed to confirm the best imaging algorithm in this small subset of patients.
