June 15, 2022
MRI, CT, and ultrasound identify blood clots not found on clinical assessment in a majority of individuals who have COVID-19 vaccine-induced low blood platelets after their first dose of the AstraZeneca vaccine, according to a case study published June 14 in Radiology.
The findings could help clinicians better care for patients who have received the AstraZeneca inoculation and have developed what is called vaccine-induced immune thrombotic thrombocytopenia (VITT), wrote a team led by Priya Rogers of Addenbrooke's Hospital in Cambridge, U.K.
"Whole-body imaging can identify patients who require early referral to specialist vascular or hepatobiliary centers [due to VITT]," the group noted.
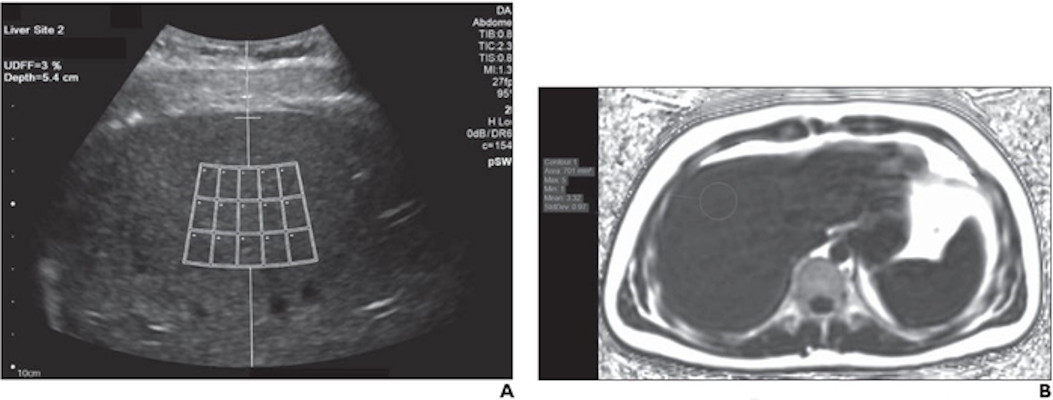
Experts recommend symptom-specific imaging for VITT, but its prevalence remains unclear, Rogers and colleagues noted. To clarify the question, the group conducted a study that included 40 patients who developed thrombocytopenia after receiving their first dose of the AstraZeneca vaccine. The patients were imaged with CT, ultrasound, and/or MRI depending on protocol in seven different centers across the U.K.
Of these 40 patients, 80% developed thrombosis symptoms within 14 days and 20% within 14 to 28 days. The investigators also found the following:
- 75% of patients underwent additional imaging, primarily with CT pulmonary angiogram or CT of the abdomen or pelvis.
- 83% of those patients who had additional imaging were found to have hidden blood clots.
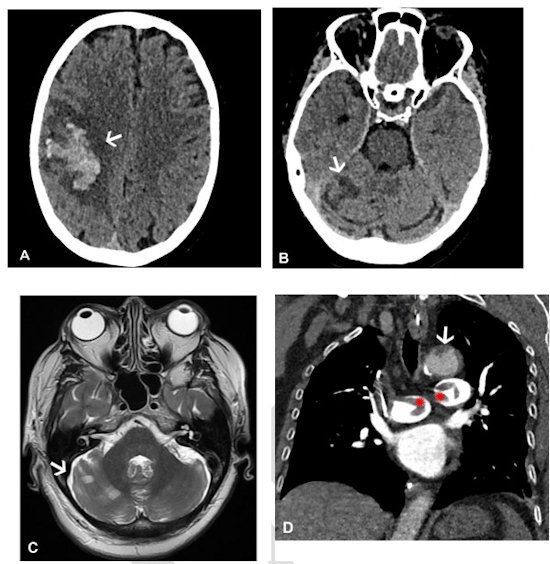
- 73% of the patient cohort presented with neurological symptoms (headache, blurred vision, seizure, collapse) and were confirmed by CT or MR venogram to have a cerebral venous sinus blood clot.
- 30% had extension of their primary blood clot.
- 20% of the total cohort died (eight of 40); those with confirmed progressive thrombosis (four patients) had a mortality rate of 50%.
Most patients underwent some form of CT imaging, the authors noted.
| Imaging modality within 48 hours of admission for symptoms of blood clotting | |||||||
| Total patients | MRI abdomen with contrast | Ultrasound duplex abdomen | Ultrasound duplex peripheral veins | CT abdomen/pelvis with contrast | CT pulmonary angiogram | CT chest abdomen/pelvis with contrast/CT aortogram | CT head and CT/MRI venogram |
| 40 | 1 | 1 | 1 | 9 | 15 | 15 | 39 |
Imaging can play a key role in identifying and dealing with vaccine complications, according to Rogers and colleagues.
"[Our] findings emphasize that VITT is a multisystem disorder and suggest that whole-body contrast-enhanced imaging is likely to identify further thrombosis," they concluded.