Tổng số lượt xem trang
Thứ Sáu, 13 tháng 6, 2014
NHÂN CA NANG CỦA SỤN TUYẾN GIÁP TẠI MEDIC
Bệnh nhân nam 33 tuổi khám kiểm tra vùng cổ, được bs Phạm thị Thanh Xuân ở phòng Siêu âm Trung tâm Medic, phát hiện có 1 nang nhỏ trong sụn giáp bên P, kích thước = 8x7mm.
Siêu âm đàn hồi ARFI xác nhân là cấu trúc nang trong sụn giáp, với VTI= brighter color (mềm) và VTQ=1,5m/s.
Kết luận là nang sụn giáp P.
Y văn chưa thấy mô tả siêu âm nang sụn giáp, có bài về CT xác chẩn khối thanh quản là dystrophic ossifications của sụn giáp.
Thứ Tư, 11 tháng 6, 2014
DASH and Incisional Hernias
US Good Alternative to CT for Characterizing Incisional Hernias: Study
By James E. Barone MD
June 03, 2014
NEW YORK (Reuters Health) - Using dynamic abdominal sonography to measure incisional hernias is equivalent to using computerized tomography (CT), according to a new study.
As opposed to a CT scan, dynamic abdominal sonography for hernia (DASH) is a bedside procedure, its results are available immediately and it does not use ionizing radiation, researchers write in JAMA Surgery, online May 28.
"The DASH examination is a feasible and accurate method for evaluating hernias, particularly in those patients who have smaller hernias and who may have unclear physical exam findings," lead author Dr. Rebeccah B. Baucom from Vanderbilt University Medical Center in Nashville, Tennessee, told Reuters Health by email.
A previous paper by Dr. Baucom and colleagues showed that CT was better at detecting incisional hernias than physical examination by surgeons. In another study, the team found that DASH was as accurate as CT scan in diagnosing hernias.
To see if DASH could be used to plan operative procedures using measurements of hernia defect size, the researchers compared it with CT scans in 109 patients. One surgeon performed all of the DASH examinations, whereas one of three surgeons read the CT scans.
The mean patient BMI was 32.2, and 34% of the patients had at least one previous hernia repair.
As measured by CT, the mean surface area of hernias was 44.6 cm2, compared to 41.8 cm2 with DASH (p=0.82). The transverse dimensions were nearly identical at 5.20 cm for CT and 5.17 cm for DASH (p=0.71).
Measurements were comparably accurate for CT scan and DASH among the 14 morbidly obese patients (BMI>39.9), 49 who were obese (BMI 30 to 39.9), and 46 who had a BMI under 30.
The authors also looked at the subgroup of hernias that were 10 cm or larger in transverse dimension. Of the 15 patients in that category, the mean surface area of the hernias was 189.4 cm2 by CT and 171.3 cm2 by DASH, an insignificant difference (p=0.26).
"Several of our surgeons perform DASH examinations on their patients who present with suspected incisional hernias," said Dr. Baucom, adding that it is also being done more and more often at follow-ups after repair.
Dr. Michael Liang, who has studied ventral hernia repair but was not involved in the new work, said, "DASH is a safe and potentially effective modality for the surgeon to use to assess ventral incisional hernias."
But Dr. Liang, of the University of Texas Health Sciences Center at Houston, raised a number of concerns about the study. For example, he told Reuters Health, the authors did not use operative findings, the gold standard, to validate the ultrasound and CT results, nor did they adjust for the size of the hernias.
For recurrent, large, and complex ventral hernias, Dr. Liang said a CT scan will be obtained regardless of DASH availability because the former modality "is useful to assess defect size, peritoneal volume, lateral muscles, abdominal wall thickness and contraction, intra-abdominal organs, and old mesh."
According to Dr. Baucom and colleagues, however, DASH plus physical examination have been sufficient to evaluate most of these structures and relationships.
SOURCE: http://bit.ly/1nZk6EV
JAMA Surgery 2014.
By James E. Barone MD
June 03, 2014
NEW YORK (Reuters Health) - Using dynamic abdominal sonography to measure incisional hernias is equivalent to using computerized tomography (CT), according to a new study.
As opposed to a CT scan, dynamic abdominal sonography for hernia (DASH) is a bedside procedure, its results are available immediately and it does not use ionizing radiation, researchers write in JAMA Surgery, online May 28.
"The DASH examination is a feasible and accurate method for evaluating hernias, particularly in those patients who have smaller hernias and who may have unclear physical exam findings," lead author Dr. Rebeccah B. Baucom from Vanderbilt University Medical Center in Nashville, Tennessee, told Reuters Health by email.
A previous paper by Dr. Baucom and colleagues showed that CT was better at detecting incisional hernias than physical examination by surgeons. In another study, the team found that DASH was as accurate as CT scan in diagnosing hernias.
To see if DASH could be used to plan operative procedures using measurements of hernia defect size, the researchers compared it with CT scans in 109 patients. One surgeon performed all of the DASH examinations, whereas one of three surgeons read the CT scans.
The mean patient BMI was 32.2, and 34% of the patients had at least one previous hernia repair.
As measured by CT, the mean surface area of hernias was 44.6 cm2, compared to 41.8 cm2 with DASH (p=0.82). The transverse dimensions were nearly identical at 5.20 cm for CT and 5.17 cm for DASH (p=0.71).
Measurements were comparably accurate for CT scan and DASH among the 14 morbidly obese patients (BMI>39.9), 49 who were obese (BMI 30 to 39.9), and 46 who had a BMI under 30.
The authors also looked at the subgroup of hernias that were 10 cm or larger in transverse dimension. Of the 15 patients in that category, the mean surface area of the hernias was 189.4 cm2 by CT and 171.3 cm2 by DASH, an insignificant difference (p=0.26).
"Several of our surgeons perform DASH examinations on their patients who present with suspected incisional hernias," said Dr. Baucom, adding that it is also being done more and more often at follow-ups after repair.
Dr. Michael Liang, who has studied ventral hernia repair but was not involved in the new work, said, "DASH is a safe and potentially effective modality for the surgeon to use to assess ventral incisional hernias."
But Dr. Liang, of the University of Texas Health Sciences Center at Houston, raised a number of concerns about the study. For example, he told Reuters Health, the authors did not use operative findings, the gold standard, to validate the ultrasound and CT results, nor did they adjust for the size of the hernias.
For recurrent, large, and complex ventral hernias, Dr. Liang said a CT scan will be obtained regardless of DASH availability because the former modality "is useful to assess defect size, peritoneal volume, lateral muscles, abdominal wall thickness and contraction, intra-abdominal organs, and old mesh."
According to Dr. Baucom and colleagues, however, DASH plus physical examination have been sufficient to evaluate most of these structures and relationships.
SOURCE: http://bit.ly/1nZk6EV
JAMA Surgery 2014.
Thứ Hai, 9 tháng 6, 2014
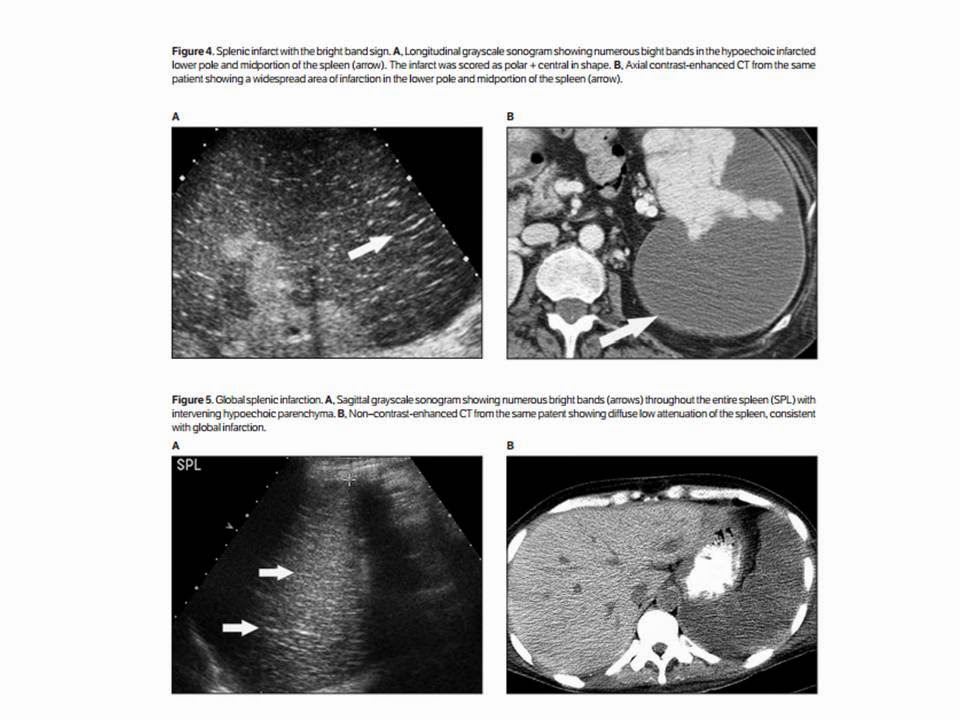
BRIGHT BAND SIGN in SPLENIC INFARCTION
In summary, the bright band sign was apparent in 91.9% of patients with splenic infarcts, including 95.7%
of those with nonclassic sonographic features of splenic infarction, was not present in a collection of 19 abnormal control patients, and was not seen in 100 normal control patients.
The bright band sign likely results from specular reflections returned from fibrous trabeculae that remain intact within infarcted regions while the neighboring splenic parenchyma undergoes necrosis. Although further work will be required to establish the role that the bright band sign may play inthe diagnosis of splenic infarction, the sign appears potentially useful, particularly for the many infarcts with nonclassic, nonspecific sonographic appearances.
Thứ Sáu, 6 tháng 6, 2014
ULTRASOUND GUIDELINES CATCHES INCIDENTAL THYROID CANCERS
In a retrospective 10-year review, a team led by Dr. Manisha Bahl from Duke University Medical Center found that adopting SRU guidelines for follow-up of incidental thyroid nodules would result in only 2% of thyroid cancers being missed. In addition, the missed tumors tended to be much smaller and more likely to be stage I than those found during workup recommended by the SRU guidelines.
"When the SRU criteria-negative incidental cancers are compared to SRU criteria-positive incidental cancers, they are smaller in size, more likely to be papillary carcinoma, and less likely to have nodal metastases," senior author Dr. Jenny Hoang told AuntMinnie.com. "In general, these characteristics belong to thyroid cancers that are more likely to have an indolent course and may never become symptomatic in the patient's lifetime."
A big problem
Incidental thyroid nodules spotted on ultrasound and other imaging modalities are a big healthcare problem in the U.S.: The nodules are common and workup can lead to patient anxiety and unnecessary and costly procedures or surgery, Hoang said.
Guidelines such as SRU's thyroid recommendations are important in reducing the growing number of biopsies being performed for incidental thyroid nodules. However, the SRU recommendations -- which were published in 2005 -- have not been widely adopted by clinicians and radiologists, including those at Duke, she said.
A previous Duke study found that using SRU recommendations could prevent 30% of biopsies. However, that study population consisted mostly of benign nodules "and did not adequately address the fear of missing more cancers in a larger cohort of patients with incidental thyroid nodules over time," she said. "In this paper we specifically addressed that fear: How many incidental cancers would be missed with the SRU recommendations over a decade?"
The group retrospectively reviewed data from thyroid surgery patients from January 1, 2003, through December 31, 2012. After evaluating imaging studies and reports for incidental thyroid nodules, the team categorized incidental nodules using the SRU criteria to ascertain the characteristics of malignant nodules that would and would not have been worked up (Radiology, June 2014, Vol. 271:3, pp. 888-894).
Of the 2,090 thyroid surgery patients included in the study, 680 were found to have thyroid cancer; 101 (15%) had incidental thyroid nodules detected on imaging. After the researchers applied the SRU recommendations to the 90 patients who had available ultrasound images or reports, they determined that 16 (18% of the 90 patients and 2% of all thyroid cancers) would have been missed using the criteria.
The tumors that would not have been worked up under the SRU criteria had a mean size of 1.1 cm (range, 0.9-1.4 cm), compared with a mean size of 2.5 cm (range, 1.0-7.6 cm) for those that had met the SRU recommendations. The difference was statistically significant (p < 0.001). Nearly all (15/16, 94%) were stage I, compared with 47 (64%) of the 74 incidental thyroid nodules that met the SRU criteria.
Fourteen (88%) of the 16 SRU criteria-negative cancers were papillary carcinoma; small papillary carcinoma has an extremely high survival rate. The other cases were a follicular carcinoma and a medullary carcinoma.
Transverse ultrasound image of an SRU criteria-negative thyroid cancer. Incidentally detected at CT, this 1.2-cm thyroid nodule is solid in composition. It does not meet the SRU recommendations for fine-needle aspiration biopsy. The postsurgical pathologic result was papillary cancer. Image courtesy of Dr. Manisha Bahl.
The researchers were surprised to find that patients with incidental thyroid cancers only represented 15% of patients who had surgery for thyroid cancer, Hoang said. The group's two prior studies had found that 29% of patients with incidental thyroid nodules underwent ultrasound-guided biopsy and 23% of patients had thyroid surgery for nodules.
"The overall lower proportion of incidental thyroid cancers among all thyroid cancer patients simply highlights the fact that benign incidental thyroid nodules are common, but cancer among the incidental nodules is uncommon," she said.
For practicing radiologists and clinicians, the clinical implication from this study and the group's prior studies is that SRU recommendations "can be used to better manage workup of incidental thyroid nodules and that SRU recommendations achieve the goal of ensuring that clinically important thyroid cancers would undergo biopsy, while avoiding unnecessary tests and surgery in patients with benign nodules," Hoang said.
Adoption of guidelines
In addition to SRU, the American Association of Clinical Endocrinologists (AACE) and the American Thyroid Association (ATA) have guidelines that recommend fine-needle aspiration (FNA) biopsy of thyroid nodules based on ultrasound findings. When speaking with a number of radiologists from different practice types over the past couple years, Hoang was most commonly told that the clinician decides which nodules receive biopsies.
"Most clinicians use a size cutoff of 1 cm for solid nodules which is part of the AACE and ATA guidelines," she said. "This is seemingly a small difference compared to the SRU 1.5-cm cutoff [for nodules without microcalcification], but another study from our group showed that one in four biopsies could be prevented with the SRU recommendations. Therefore, increasing the size cutoff by just 5 mm can substantially reduce the proportion of thyroid nodules that require biopsy."
Hoang said that she hopes this study will encourage more widespread adoption of the SRU recommendations.
"Radiologists and clinicians now have our study to allay fears of missing many and significant cancers by being more selective in the workup of incidental thyroid nodules," she said.
Hoang also noted that she is a member of an American College of Radiology (ACR) committee that will produce a white paper in the coming year on incidental thyroid nodules for all imaging modalities. Furthermore, Duke has developed a three-tier system for reporting incidental thyroid nodules found on CT, MRI, or PET/CT, she said.
"When the SRU criteria-negative incidental cancers are compared to SRU criteria-positive incidental cancers, they are smaller in size, more likely to be papillary carcinoma, and less likely to have nodal metastases," senior author Dr. Jenny Hoang told AuntMinnie.com. "In general, these characteristics belong to thyroid cancers that are more likely to have an indolent course and may never become symptomatic in the patient's lifetime."
A big problem
Incidental thyroid nodules spotted on ultrasound and other imaging modalities are a big healthcare problem in the U.S.: The nodules are common and workup can lead to patient anxiety and unnecessary and costly procedures or surgery, Hoang said.
Guidelines such as SRU's thyroid recommendations are important in reducing the growing number of biopsies being performed for incidental thyroid nodules. However, the SRU recommendations -- which were published in 2005 -- have not been widely adopted by clinicians and radiologists, including those at Duke, she said.
A previous Duke study found that using SRU recommendations could prevent 30% of biopsies. However, that study population consisted mostly of benign nodules "and did not adequately address the fear of missing more cancers in a larger cohort of patients with incidental thyroid nodules over time," she said. "In this paper we specifically addressed that fear: How many incidental cancers would be missed with the SRU recommendations over a decade?"
The group retrospectively reviewed data from thyroid surgery patients from January 1, 2003, through December 31, 2012. After evaluating imaging studies and reports for incidental thyroid nodules, the team categorized incidental nodules using the SRU criteria to ascertain the characteristics of malignant nodules that would and would not have been worked up (Radiology, June 2014, Vol. 271:3, pp. 888-894).
Of the 2,090 thyroid surgery patients included in the study, 680 were found to have thyroid cancer; 101 (15%) had incidental thyroid nodules detected on imaging. After the researchers applied the SRU recommendations to the 90 patients who had available ultrasound images or reports, they determined that 16 (18% of the 90 patients and 2% of all thyroid cancers) would have been missed using the criteria.
The tumors that would not have been worked up under the SRU criteria had a mean size of 1.1 cm (range, 0.9-1.4 cm), compared with a mean size of 2.5 cm (range, 1.0-7.6 cm) for those that had met the SRU recommendations. The difference was statistically significant (p < 0.001). Nearly all (15/16, 94%) were stage I, compared with 47 (64%) of the 74 incidental thyroid nodules that met the SRU criteria.
Fourteen (88%) of the 16 SRU criteria-negative cancers were papillary carcinoma; small papillary carcinoma has an extremely high survival rate. The other cases were a follicular carcinoma and a medullary carcinoma.
Transverse ultrasound image of an SRU criteria-negative thyroid cancer. Incidentally detected at CT, this 1.2-cm thyroid nodule is solid in composition. It does not meet the SRU recommendations for fine-needle aspiration biopsy. The postsurgical pathologic result was papillary cancer. Image courtesy of Dr. Manisha Bahl.
The researchers were surprised to find that patients with incidental thyroid cancers only represented 15% of patients who had surgery for thyroid cancer, Hoang said. The group's two prior studies had found that 29% of patients with incidental thyroid nodules underwent ultrasound-guided biopsy and 23% of patients had thyroid surgery for nodules.
"The overall lower proportion of incidental thyroid cancers among all thyroid cancer patients simply highlights the fact that benign incidental thyroid nodules are common, but cancer among the incidental nodules is uncommon," she said.
For practicing radiologists and clinicians, the clinical implication from this study and the group's prior studies is that SRU recommendations "can be used to better manage workup of incidental thyroid nodules and that SRU recommendations achieve the goal of ensuring that clinically important thyroid cancers would undergo biopsy, while avoiding unnecessary tests and surgery in patients with benign nodules," Hoang said.
Adoption of guidelines
In addition to SRU, the American Association of Clinical Endocrinologists (AACE) and the American Thyroid Association (ATA) have guidelines that recommend fine-needle aspiration (FNA) biopsy of thyroid nodules based on ultrasound findings. When speaking with a number of radiologists from different practice types over the past couple years, Hoang was most commonly told that the clinician decides which nodules receive biopsies.
"Most clinicians use a size cutoff of 1 cm for solid nodules which is part of the AACE and ATA guidelines," she said. "This is seemingly a small difference compared to the SRU 1.5-cm cutoff [for nodules without microcalcification], but another study from our group showed that one in four biopsies could be prevented with the SRU recommendations. Therefore, increasing the size cutoff by just 5 mm can substantially reduce the proportion of thyroid nodules that require biopsy."
Hoang said that she hopes this study will encourage more widespread adoption of the SRU recommendations.
"Radiologists and clinicians now have our study to allay fears of missing many and significant cancers by being more selective in the workup of incidental thyroid nodules," she said.
Hoang also noted that she is a member of an American College of Radiology (ACR) committee that will produce a white paper in the coming year on incidental thyroid nodules for all imaging modalities. Furthermore, Duke has developed a three-tier system for reporting incidental thyroid nodules found on CT, MRI, or PET/CT, she said.
Thứ Năm, 5 tháng 6, 2014
ULTRASOUND MATCHES CT for KIDNEY STONE IMAGING
Ultrasound Matches CT for Kidney Stone Imaging
Neil Osterweil
May 17, 2014
ORLANDO, Florida — Ultrasound was comparable to CT in its ability to discriminate between renal calculi and other causes of flank pain, according to the results of a new study.
"Routine utilization of CT as a knee-jerk response for someone presenting with acute colic is inappropriate, not only for cost but for radiation exposure," said Marshall L. Stoller, MD, professor and vice chair of urology at the University of California, San Francisco.
More important, this study shows that using ultrasound has no adverse impact on patient outcomes, said Dr. Stoller.
The results of the study were presented here at the American Urological Association 2014 Annual Scientific Meeting.
A Multicenter Study
Dr. Stoller and colleagues at 15 academic medical centers conducted a randomized trial in which adult patients presenting to an emergency department with suspected nephrolithiasis were randomly assigned to receive point-of-care ultrasound performed by an emergency physician, ultrasound performed by a radiologist, or abdominal CT. Additional tests were at the discretion of each patient's physician.
The investigators looked at the incidence of serious adverse events diagnosed within 30 days of imaging, cumulative radiation exposure, and cost. Follow-up with detailed, structured patient interviews was done at 3 and 7 days, and again at 1, 3, and 6 months.
The incidence of serious adverse events among patients assigned to CT was 11.1%, compared with 12.3% for patients who underwent ultrasound performed by an emergency physician and 10.6% for those whose ultrasound scans were performed by a radiologist. The differences were not significant.
Severe adverse events — including abdominal aortic aneurysm with rupture, pneumonia with sepsis, appendicitis with rupture, inflammatory bowel conditions and renal infarction, pyelonephritis with urosepsis, and ovarian torsion with necrosis — occurred in 5 of 908 patients (0.55%) assigned to emergency-physician-performed ultrasound, 3 of 893 patients (0.34%) assigned to radiologist-performed ultrasound, and 4 of 958 patients (0.42%) assigned to CT.
Not surprisingly, patients who underwent ultrasound had significantly lower average cumulative radiation exposures, at 10.5 mSv and 9.3 mSv for emergency-physician- and radiologist-performed ultrasound, respectively, compared with 17 mSv for patients who underwent CT (P < .0001).
There were no significant differences in hospital readmissions after discharge, average pain scores, pain resolution, or subsequent serious adverse events, the investigators found.
Average imaging costs were about 33% to 50% higher for CT (average, $300) than for ultrasound ($150 if done by an emergency physician, and $200 if done by a radiologist).
Concerns About Radiation
This study shows that emergency department physicians need not fear missing a diagnosis of kidney stones or other causes of acute pain if they choose ultrasound over CT as an initial imaging modality, said Margaret Pearle, MD, PhD, professor of urology at the University of Texas Southwestern Medical Center at Dallas and the Center for Mineral Metabolism and Clinical Research.
And patients can be confident that their chance of getting an accurate diagnosis is comparable, she added.
"I think in our institution, probably like the majority of institutions, if someone comes in with acute flank pain, the first test is a CT, although we're starting to see a little bit of a trend toward ultrasound," Dr. Pearle told Medscape Medical News.
The shift appears to be driven more by patient and clinician concerns about radiation exposure, rather than administrative worries over cost, she said.
"There's tremendous fear right now, particularly on the part of patients. They hear that radiation exposure is bad, and they don't [want to be exposed]," she said. "Stone disease is one of those conditions that is associated with repeated imaging studies because of repeated symptomatic episodes."
Dr. Pearle was not involved in the study.
Because of fragmentation and lack of coordination of healthcare, some patients get repeat exposure to ionizing radiation for the same episode of pain, said Dr. Stoller.
"It is not uncommon in my clinic that you'll see someone in their 20s coming in with 5 or 6 CTs from the past week or 2. That's a huge amount of radiation," he said.
The study was supported by the National Institutes of Health. Dr. Stoller and Dr. Pearle have reported no relevant financial relationships.
American Urological Association (AUA) 2014 Annual Scientific Meeting. Abstract PD4-03. Presented May 16, 2014.
Neil Osterweil
May 17, 2014
ORLANDO, Florida — Ultrasound was comparable to CT in its ability to discriminate between renal calculi and other causes of flank pain, according to the results of a new study.
"Routine utilization of CT as a knee-jerk response for someone presenting with acute colic is inappropriate, not only for cost but for radiation exposure," said Marshall L. Stoller, MD, professor and vice chair of urology at the University of California, San Francisco.
More important, this study shows that using ultrasound has no adverse impact on patient outcomes, said Dr. Stoller.
The results of the study were presented here at the American Urological Association 2014 Annual Scientific Meeting.
A Multicenter Study
Dr. Stoller and colleagues at 15 academic medical centers conducted a randomized trial in which adult patients presenting to an emergency department with suspected nephrolithiasis were randomly assigned to receive point-of-care ultrasound performed by an emergency physician, ultrasound performed by a radiologist, or abdominal CT. Additional tests were at the discretion of each patient's physician.
The investigators looked at the incidence of serious adverse events diagnosed within 30 days of imaging, cumulative radiation exposure, and cost. Follow-up with detailed, structured patient interviews was done at 3 and 7 days, and again at 1, 3, and 6 months.
The incidence of serious adverse events among patients assigned to CT was 11.1%, compared with 12.3% for patients who underwent ultrasound performed by an emergency physician and 10.6% for those whose ultrasound scans were performed by a radiologist. The differences were not significant.
Severe adverse events — including abdominal aortic aneurysm with rupture, pneumonia with sepsis, appendicitis with rupture, inflammatory bowel conditions and renal infarction, pyelonephritis with urosepsis, and ovarian torsion with necrosis — occurred in 5 of 908 patients (0.55%) assigned to emergency-physician-performed ultrasound, 3 of 893 patients (0.34%) assigned to radiologist-performed ultrasound, and 4 of 958 patients (0.42%) assigned to CT.
Not surprisingly, patients who underwent ultrasound had significantly lower average cumulative radiation exposures, at 10.5 mSv and 9.3 mSv for emergency-physician- and radiologist-performed ultrasound, respectively, compared with 17 mSv for patients who underwent CT (P < .0001).
There were no significant differences in hospital readmissions after discharge, average pain scores, pain resolution, or subsequent serious adverse events, the investigators found.
Average imaging costs were about 33% to 50% higher for CT (average, $300) than for ultrasound ($150 if done by an emergency physician, and $200 if done by a radiologist).
Concerns About Radiation
This study shows that emergency department physicians need not fear missing a diagnosis of kidney stones or other causes of acute pain if they choose ultrasound over CT as an initial imaging modality, said Margaret Pearle, MD, PhD, professor of urology at the University of Texas Southwestern Medical Center at Dallas and the Center for Mineral Metabolism and Clinical Research.
And patients can be confident that their chance of getting an accurate diagnosis is comparable, she added.
"I think in our institution, probably like the majority of institutions, if someone comes in with acute flank pain, the first test is a CT, although we're starting to see a little bit of a trend toward ultrasound," Dr. Pearle told Medscape Medical News.
The shift appears to be driven more by patient and clinician concerns about radiation exposure, rather than administrative worries over cost, she said.
"There's tremendous fear right now, particularly on the part of patients. They hear that radiation exposure is bad, and they don't [want to be exposed]," she said. "Stone disease is one of those conditions that is associated with repeated imaging studies because of repeated symptomatic episodes."
Dr. Pearle was not involved in the study.
Because of fragmentation and lack of coordination of healthcare, some patients get repeat exposure to ionizing radiation for the same episode of pain, said Dr. Stoller.
"It is not uncommon in my clinic that you'll see someone in their 20s coming in with 5 or 6 CTs from the past week or 2. That's a huge amount of radiation," he said.
The study was supported by the National Institutes of Health. Dr. Stoller and Dr. Pearle have reported no relevant financial relationships.
American Urological Association (AUA) 2014 Annual Scientific Meeting. Abstract PD4-03. Presented May 16, 2014.
Đăng ký:
Bài đăng
(
Atom
)