In conclusion, assessment of blood leukocyte counts at hospital admission in patients with CAP virtually rule out COVID-19 in those cases with basophils and eosinophils greater than 17 and 10 cells/mm3, respectively. Our findings will help to optimize the triage of patients with pneumonia pending the results of NAAT and they will also help to improve the management of false negative results on the first NPS.
Tổng số lượt xem trang
Thứ Sáu, 10 tháng 9, 2021
BLOOD CELL COUNT and L U S Ruling out COVID-19 in Patients with Pneumonia
In conclusion, assessment of blood leukocyte counts at hospital admission in patients with CAP virtually rule out COVID-19 in those cases with basophils and eosinophils greater than 17 and 10 cells/mm3, respectively. Our findings will help to optimize the triage of patients with pneumonia pending the results of NAAT and they will also help to improve the management of false negative results on the first NPS.
Thứ Hai, 6 tháng 9, 2021
Role of Lung Ultrasound in Patients with Severe COVID-19 in Low and Middle-Income Countries [LMICs]
In LMICs,
what is the role of lung ultrasound in patients with severe COVID-19? Rationale.
Chest imaging can be essential in the diagnosis and
management of patients with COVID-19. Published reports to date have focused
mainly on standard chest x-ray (CXR) and chest computed tomography (CT).
Abnormalities are very often present on CXR images of COVID-19 patients44;
consolidations and ground-glass opacities have been reported in 47% and 33%,
respectively. Not all patients with COVID-19 have abnormalities on chest CT
images.45 Patchy ground-glass opacities, typically in a bilateral and
peripheral locations, and consolidations have been most commonly
described.46–48 In light of the high sensitivity of an abnormal scan, CT has
even been suggested as a primary diagnostic tool for COVID-19.49,50 Challenges
with access to CT and, at times, even simple CXR may preclude the usefulness of
these imaging techniques in LMICs.
Lung ultrasound (LUS) is increasingly recognized as a chest
imaging tool with a strong potential to guide management of critically ill
patients and may represent a useful tool in patients with COVID-19. Search
results. MEDLINE, Embase, and Web of Science were searched until May 2020. The
search used combinations of MeSH terms and free-text words, including
“COVID–19,” “coronavirus,” “SARS–CoV–2,” “‘radiography,” “chest radiography,”
“CT,” “chest CT,” “CT,” “chest CT,” “ultrasound,” “LUS,” and “lung
ultrasonography.” Several studies were found but none reporting data from
LMICs.
Evidence. For the diagnosis of pneumonia from causes other than COVID-19, LUS has been found to be superior to standard CXR, and it approaches chest CT in terms of diagnostic accuracy.51–53 Lung ultrasound had a better diagnostic yield than CXR in the early diagnosis of H1N1 2009 viral pneumonia.54 Experience with LUS in patients with COVID-19 is rapidly growing, with the consistent finding that nearly all COVID-19 patients have an abnormal LUS.55
Four major findings are frequently
described in COVID-19 patients (Figure 1), although the sensitivity and
specificity of the following findings remain uncertain.56
1. focal, multifocal,
or confluent B-lines (in 97% of cases);
2. pleural thickening
(in 50% of cases);
3. subpleural and
pleural consolidations (in 40% of cases); and
4. rarely, pleural effusions (in 16% of cases).57–61 A patchy distribution of multiform clusters alternating with “spared areas” (regions of normal lung parenchyma) is often observed.62
One LUS finding of particular usefulness in COVID-19 is the “light
beam,” a broad, lucent, band-shaped, vertical artifact that moves rapidly with
sliding (see https:// link.springer.com/article/10.1007/s00134-020-06048-9),
which may correspond to early ground-glass alterations on a chest CT scan. The
precise diagnostic accuracy of this sign is currently being tested in a
prospective study.63 Early reports suggest that the extent of LUS findings
correlate with severity of lung injury in COVID-19.45 In one review of LUS in
patients with COVID-19, the relative number and distribution of B-lines and
consolidations approximated other parameters of clinical severity, including
oxygen saturation, need for supplemental oxygenation, and respiratory rate.64
The WHO clinical management guidelines suggest that LUS be used to assist in
COVID-19 diagnosis and identify or exclude pulmonary complications.1
Potentially useful scoring systems for patients with COVID19 are summarized in
Table 2. A scoring system to quantify the degree of lung injury in patients
with COVID-19 has been proposed for both ventilated and non-ventilated patients
(Figure 1).65 In invasively ventilated patients, early quantification of the
severity of lung involvement by LUS in patients with COVID-19 can be estimated
by using the “LUS score,” 66 which has been extensively tested in ARDS
patients.67,68 The dynamic changes in aeration can then potentially be
quantified by reassessing the LUS score (Figure 2). A previous study in Rwanda
proposed the use of LUS combined with pulse oximetry to diagnose ARDS (from
causes other than COVID19) in a cohort of primarily non-ventilated patients.69
This approach was externally validated in invasively ventilated patients in the
Netherlands,70 but its performance in COVID19 ARDS remains to be established.
To our knowledge, there are currently no published studies comparing LUS with
RT-PCR for the diagnosis of COVID-19. However, multiple studies looking at
diagnosis (NCT0435180, NCT04370275, NCT04393402, NCT04338568, NCT04322487, and
NCT04377035) or prognosis (NCT04379544, NCT04384055, and NCT04370249) are
currently underway as of November 5, 2020. One of these studies is being
performed in Turkey (NCT04399681). Availability, feasibility, affordability,
and safety. Data on the availability of ultrasound devices in LMICs remain
limited. In a recent multicenter observational study in 54 Asian ICUs, 54% of
centers reported having a dedicated chest radiography apparatus versus 79% an
ultrasound apparatus,71 and a hospital CT was available in 96% of centers. A
bedside ultrasound machine was reported to be available sometimes in Haiti.72
Lung ultrasound studies in LMICs are still performed less frequently than
abdominal and cardiac ultrasound.73 However, with the availability of smaller
and cheaper devices and a growing body of evidence, wider use of LUS can be foreseen.74,75
Although cost-effectiveness studies in LMICs are lacking, LUS has been shown to
reduce the use of CXR and chest CT in resource-rich ICUs, with less radiation
exposure and lower costs.76,77 An important advantage of LUS is that it can be
performed with most available ultrasound machines and probes. It remains an
operator-dependent technique but can be taught readily to non-experts with
little formal ultrasonography training. In an international, multicenter study
across 10 ICUs, performance of 25 supervised LUS examinations resulted in
sufficient acquisition of skills by non-experts for the assessment of the “LUS
score.” 78 In more resource-restricted settings, a study of 20 participants in
Ghana demonstrated good retention of cardiorespiratory ultrasonography
principles 9– 11 months after participants received a training program.79
Point-of-care ultrasound training intervention in a resource restricted setting
in Rwanda resulted in high numbers of diagnostic quality studies over long-term
follow-up,80,81 although remote quality assurance feedback was found an
effective educational tool in Uganda.
An important limitation of LUS is that it cannot detect lesions that are intrapulmonary and do not reach the pleural line.82 Usefulness of LUS via telemedicine is proposed, but direct evidence is still lacking.83
Recommendations and suggestions (Table 1).
1. In LMICs, where availability of standard CXR and CT is limited, we suggest using LUS to detect abnormalities to identify patients with possible COVID-19 (weak recommendation, low quality of evidence);
2. In LMICs, we recommend against the use of LUS to exclude COVID-19 (UG best practice statement);
3. In LMICs, we suggest using LUS in combination
with clinical parameters to monitor progress of the disease and responses to
therapy in COVID-19 patients (weak recommendation, low quality of evidence).
LMICs= Low and Middle-Income Countries
-----------
Thứ Bảy, 4 tháng 9, 2021
Thứ Sáu, 3 tháng 9, 2021
US scoring index shows promise in COVID diagnosis
By Amerigo Allegretto, AuntMinnie.com staff writer
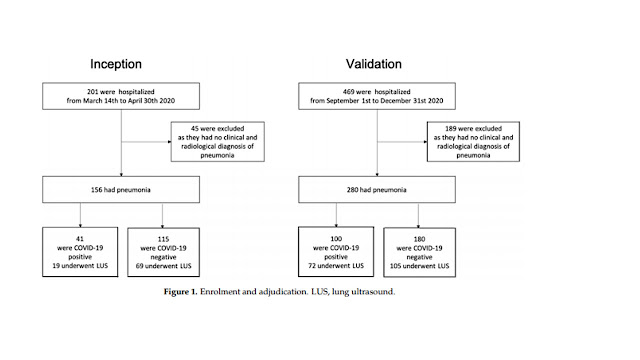
September 3, 2021 -- A novel ultrasound scoring system that can be performed in less than 10 minutes is accurate for COVID-19 diagnosis and prognosis, according to research published August 31 in Ultrasound in Medicine and Biology.
A team led by Dr. Michele Spampinato from the University of Ferrara in Italy said that their lung ultrasound severity index could distinguish between patients who have COVID-19 and those who don't. It also can better identify patients who will experience in-hospital mortality when compared with standard lung ultrasound severity scores.
"In such an epidemiological scenario, in which a huge number of patients are admitted for the same disease, early differentiation of patients with highly infectious disease from patients with other causes of respiratory distress is essential," Spampinato and colleagues wrote.
Chest imaging has been a primary method of diagnosing and evaluating the severity of COVID-19, with ultrasound being touted as easily accessible and not exposing patients to radiation. However, studies are generally based on score systems that do not consider the patchy ultrasound appearance of SARS-CoV-2 pneumonia. The researchers said this is due to the different patterns displayed in the same area.
"In our opinion, this issue could be relevant to better assess lung ultrasound diagnostic characteristics in SARS-CoV-2 pneumonia," they added.
Spampinato et al created their lung ultrasound severity index to better describe the coexistence of different lung lesions in the same lung area. This in turn can be used to measure the quality and extent of lung involvement in relation to COVID-19 diagnosis, as well as in-hospital mortality of patients with respiratory distress admitted for suspected COVID-19.
They tested the accuracy of the index in a study with 159 patients (105 male, 54 female) with an average age of 64.6 years with suspected SARS-CoV-2 pneumonia. Out of these, 63.5% were diagnosed with COVID-19.
COVID-19 patients had a higher mortality rate (18.8% vs. 6.9%) and lung ultrasound severity index score (16.14 vs. 10.08) compared with non-COVID-19 cases.
The team compared the index to several other measures, including lung ultrasound severity score, the simple sum of lung ultrasound findings, and a lung ultrasound heterogeneity score, the number of different ultrasound patterns found in each area.
| Prognostic characteristics of lung ultrasound scores for in-hospital mortality | |||
| Lung ultrasound heterogeneity score | Lung ultrasound severity score | Lung ultrasound scoring index | |
| Area under the receiver operating characteristic (AUROC) | 0.576 | 0.733 | 0.805 |
| Sensitivity | 69.57% | 65.22% | 90.91% |
| Specificity | 48.53% | 73.53% | 65.67% |
| Odds Ratio | 1.037 | 1.045 | 1.14 |
The researchers said the scoring index combines the strengths of the other two scoring methods, citing the index's higher AUROC scores. The index's AUROC score for diagnosing COVID-19 was 0.72 and 0.76 for predicting in-hospital mortality for COVID-19 patients. Both were higher than the severity and heterogeneity scores.
The team also touted the amount of time it takes to perform an ultrasound scan, which averaged 8.05 minutes, much less than the several hours it takes to get information from lab exams, swabs, and high-resolution CT. The team said by using lung ultrasound and applying the scoring index to identify high COVID-19 risk, doctors can make better decisions about further imaging, urgent therapies, and a patient's destination.
Spampinato and colleagues called for more validation studies for lung ultrasound scoring with large patient populations, different clinical settings, and comparison with other imaging methods.
"Researchers should make every effort to reach an agreement on a standard of reference in the conducting, reporting, and grading pulmonary involvement in SARS-CoV-2 pneumonia," the study authors wrote.