March 26, 2020 -- Ultrasound artificial intelligence software and simulation developer Intelligent Ultrasound Group has released a COVID-19 training module free of charge to hospitals in the U.S. and the U.K.
Tổng số lượt xem trang
Thứ Năm, 26 tháng 3, 2020
Intelligent Ultrasound offers COVID-19 training module.
By AuntMinnie.com staff writers
March 26, 2020 -- Ultrasound artificial intelligence software and simulation developer Intelligent Ultrasound Group has released a COVID-19 training module free of charge to hospitals in the U.S. and the U.K.
March 26, 2020 -- Ultrasound artificial intelligence software and simulation developer Intelligent Ultrasound Group has released a COVID-19 training module free of charge to hospitals in the U.S. and the U.K.
Thứ Ba, 24 tháng 3, 2020
Doctor in Italy, Spain using ultrasound for COVID-19
By Theresa Pablos, AuntMinnie staff writer
The first day after Chen's diagnosis he experienced a sore throat, dry cough, and headache but no lung ultrasound abnormalities. All videos courtesy of Dr. Yale Tung Chen.
By the fourth day following his diagnosis, Chen's ultrasound scan on his left side showed an increasingly thickened pleural line and two subpleural consolidations.
On the 12th day after his diagnosis, Chen was feeling better, primarily experiencing a cough, nausea, and diarrhea. His ultrasound scans showed his subpleural consolidations were resolving, but he still had thickened pleura and B-lines, as well as a small effusion.
March 23, 2020 -- As Europe struggles to cope with the novel coronavirus outbreak, one doctor in Spain is using point-of-care ultrasound (POCUS) to track his own COVID-19 disease. His findings echo those of other doctors on the front lines in showing that ultrasound can help with diagnosis, treatment, and admission decisions.
Dr. Yale Tung Chen, an emergency medicine physician at an academic hospital in Madrid, was diagnosed with COVID-19 following a rapid polymerase chain reaction (PCR) test on March 8. Like his patients, many of his first symptoms were mild -- a little worse than a common cold, he said during a March 19 webinar on POCUS for COVID-19.
Chen's initial lung ultrasound scans appeared normal, too. However, in the days following his positive test result, lung sliding started to appear laterally on the ultrasound scan. He also saw some B-lines and thickening of the pleura. On day four, he noticed subpleural consolidations for the first time.
"As my disease progressed, the lower back started to clear, but then other spots were affected -- especially on the lateral sides, my axillary fossa, the scapular fossa," he said.
During this time, Chen's clinical symptoms, including fatigue and cough, would improve and then worsen again. The cyclical nature of his clinical symptoms matched what he saw on the ultrasound scans.
"[Lesions] on my back started to clear up, then reappeared a couple of days later," he said. "It's something that is quite different from any other viral pneumonia that we have faced in the past."
Now that he's more than a week out from his positive test result, Chen is doing well. His oxygen saturation never dropped below 95%, and he hasn't experienced dysthymia, shortness of breath, or chest pain.
He also performed cardiac imaging every two days but didn't find anything remarkable.
Ultrasound warning signs
Chen's findings on his own lung ultrasound scans mirror the findings of doctors in other European countries. Dr. Mike Stone, former division chief of emergency ultrasound at Brigham and Women's Hospital in Boston and head of education at POCUS developer Butterfly, noticed many hospitals in Italy are using lung ultrasound as a primary or secondary modality for patients with COVID-19.
The turn to ultrasound comes from a lack of resources for other types of chest imaging, such as CT, which from the start of the outbreak has demonstrated its utility in detecting COVID-19. And because POCUS can be used bedside, it avoids concerns about spreading the virus when patients are moved to different locations.
"There are many places currently using lung ultrasound as a primary imaging modality to try and address some of these concerns," Stone said during a March 19 webinar on POCUS for COVID-19.
In a normal lung ultrasound scan, ribs and shadows are evident with a pleural line that's bright and smooth, Stone noted. There are also A-lines, which are horizontal reverberation tracks from an air-filled lung.
But patients with COVID-19 tend to also exhibit focal B-lines along with spared, normal A-lines, also known as skip areas.
"Patchy B-lines and confluent B-lines," he said. "That's a pattern that we are seeing commonly in many of the images that have been sent to us over the last several weeks."
In addition, the ultrasound scans of patients with COVID-19 show a thickened pleural line. Patients can also have subpleural consolidation or traditional consolidation.
"You've got an area of almost solid organ-appearing tissue under the pleural line," Stone said. "You've got some air bronchograms. This isn't dissimilar from what you might see in bacterial pneumonia."
In COVID-19 patients, the findings also fluctuate and reoccur, as they did for Chen. Patients can have A-lines disappear, reappear a few days later, and then disappear again. Pleural consolidation can also wax and wane, according to Stone.
Ultrasound for triage
Stone polled lung ultrasound experts in his network to see how doctors in Spain, Italy, and other countries have used ultrasound systems to triage patients. While he cautioned that no doctor should be making admission or discharge decisions based solely on ultrasound scan findings, the doctors used ultrasound in similar ways.
For areas where rapid PCR testing is available, a patient with hypoxia and a positive SARS-CoV-2 PCR test is often admitted to the hospital's COVID-19 unit, with imaging left to the discretion of the treating provider.
"What I've heard repeatedly from physicians hardest hit in Italy is that in the COVID wards, when they make rounds, they'll come in and they'll scan their lungs," Stone said. "They'll scan their heart, looking for cardiac issues. They'll scan the [inferior vena cava] collapsibility to take care of all three of those assessments at one time with the single physician."
In areas where rapid PCR testing isn't available or where tests are running low, lung ultrasound is sometimes used as a secondary screening modality after patient presentation and COVID-19 risk factors.
For instance, Stone doesn't have access to rapid PCR testing, so he has been using ultrasound for patients with labored breathing.
"That's my trigger," he said. "Even if their oxygen saturations are normal, if they're feeling short of breath, I want to take a look at their lungs. That's how I'm making that decision right now."
Similarly, when Chen's wife complained of mild throat soreness a few days ago, he couldn't get access to a PCR test. So he scanned her back with POCUS instead.
"There were B-lines with the thickened pleura," he said. "I didn't need to do anything else. That was the positive result that I was waiting for."
Some patients who appear healthy can also have "ugly" ultrasound scan results. And while clinical symptoms, including hypoxia, tachycardia, and dyspnea, can lag behind ultrasound findings, that doesn't mean every patient with concerning ultrasound results needs to be admitted.
"Admission decisions are going to be based on patients who are tremendously ill," he said. "People with hypoxia, people with increased work of breathing who look unwell -- those patients are going to be coming in kind of regardless of what their lung ultrasound shows."
Too soon?
Stone stressed that there hasn't been time to do the kind of evidence-based, prospective studies the medical profession relies on. So, some of these recommendations will be quickly outdated.
Stone is collecting data based on his own experiences and those of other doctors using all types of ultrasound imaging systems in the fight against COVID-19. And so far, it's looking like lung ultrasonography may be a helpful tool -- and it's not hard to learn.
"The good news is that lung ultrasound -- as opposed to say echocardiography -- is really easily learned," he said. "The lung surface is very accessible. There aren't these tiny windows to work with. I have taught completely naive people how to look for lung sliding, A-lines, and B-lines successfully in less than a 30- or 40-minute session. So this is not challenging to learn.
Thứ Bảy, 21 tháng 3, 2020
Thứ Năm, 19 tháng 3, 2020
US can be used for patients with COVID-19.
By Theresa Pablos, AuntMinnie staff writer
March 19, 2020 -- Ultrasound scans show promise for helping to monitor patients with COVID-19, according to a letter published on March 12 in Intensive Care Medicine. The researchers used lung ultrasonography to monitor more than a dozen patients in China with COVID-19 infections.
Because of its high sensitivity, CT is currently the imaging method of choice to diagnose and monitor patients with COVID-19. However, chest CT may also present difficulties for patients with hypoxemia and hemodynamic failure, and the enclosed environment may contribute to the spread of the coronavirus.
In the research letter, the authors found lung ultrasonography could overcome some of CT's limitations. Ultrasound may even be the better imaging choice for patients in critical condition who cannot be easily moved.
"Based upon our experience, we consider that lung ultrasonography has major utility for management of COVID-19 with respiratory involvement due to its safety, repeatability, absence of radiation, low cost, and point of care use," wrote the authors, led by Qian-Yi Peng, from the critical care department at Xiangya Hospital in Changsha, China.
COVID-19 on lung ultrasound scans
Peng and colleagues performed lung ultrasonography on 20 patients with COVID-19. They used a 12-zone examination method, which resulted in the following five characteristic findings:
- Pleural line thickening and irregularity
- Variety of B-line patterns, including focal, multifocal, and confluent
- Variety of consolidation patterns, including multifocal small, nontranslobar, and translobar with occasional mobile air bronchograms
- Visible A-lines during the recovery phase
- Rare occurrence of pleural effusions
"The observed patterns occurred across a continuum from mild alveolar interstitial pattern, to severe bilateral interstitial pattern, to lung consolidation," the authors wrote.
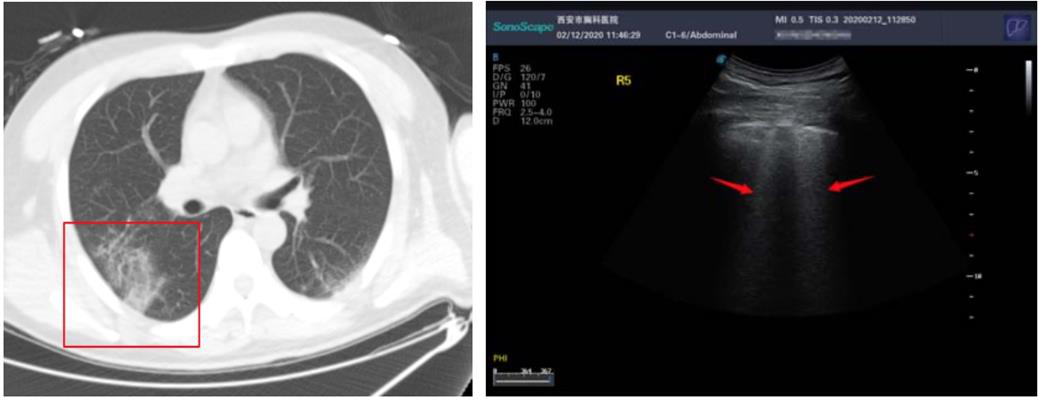
Above: A CT scan and ultrasound scan from one patient with COVID-19. Below: A CT scan and ultrasound scan from a second patient with COVID-19. All images published in SSRN and courtesy of Yi Huang and colleagues.
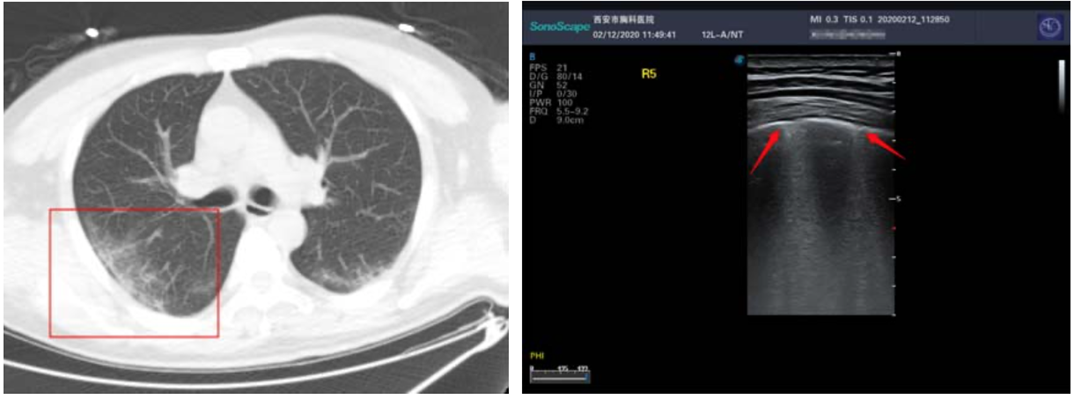
During the early stages of COVID-19, patients tended to exhibit focal B-line patterns, followed by alveolar interstitial syndrome as the disease progressed. In patients who were critically ill, ultrasound scans showed A-line patterns in the convalescence. For patients with pulmonary fibrosis, the scans found pleural line thickening with uneven B-line patterns.
"The findings of lung ultrasonography features of [COVID-19] are related to the stage of disease, the severity of lung injury, and comorbidities," the authors wrote. "The predominant pattern is of varying degrees of interstitial syndrome and alveolar consolidation, the degree of which is correlated with the severity of the lung injury."
The findings from Peng and colleagues mirror those of a previous study published on February 28 in SSRN. In the earlier study, lead author Yi Huang and colleagues used ultrasound scans for 20 patients with COVID-19 at the Xi'an Chest Hospital in Xi'an, China.
Huang and colleagues also used the 12-zone examination method and found similar ultrasound scan characteristics to Peng and colleagues. For instance, they found a higher proportion of B-line patterns in lesion areas, including fused B lines, as well as pleural lines that presented as discontinuous, interrupted, or unsmooth.
Better than CT?
The ultrasound scan findings from both studies lined up well with chest CT scans results. For instance, in Peng and colleague's study thickened pleura on CT scans presented as a thickened pleural line on ultrasound. Further, pulmonary infiltrating shadow on CT was linked to confluent B-line patterns on ultrasound.
Similarly, the chest CT scan of one patient in Huang and colleague's study showed ground-glass opacity and air bronchogram sign under the pleura of one lung (Figure 1). The ultrasound scan of the same patient revealed an uneven pleural line and B-line patterns (Figure 2).
While both sets of authors agreed that lung ultrasonography had several benefits over chest CT for patients with COVID-19, they also noted ultrasound shouldn't be used as the only imaging method. For instance, CT is still needed to identify patients who have pneumonia that does not extend to the pleural cavity,
- "Our study indicated that ultrasound can show typical manifestations and has advantages over CT in the clinical diagnosis and treatment of noncritical COVID-19, but it cannot replace CT," wrote Huang and colleagues. "Ultrasound can be used as a supplemental method."
Thứ Tư, 18 tháng 3, 2020
What US scoring system works best in diabetes?
By Theresa Pablos, AuntMinnie staff writer
March 18, 2020 -- Only one technique to assess medial arterial calcification (MAC) from an ultrasound scan can also predict related cardiovascular and diabetes complications, according to a study published on March 6 in Ultrasound in Medicine and Biology.
The authors evaluated two methods for diagnosing MAC severity:
- The presence of MAC in three unique artery segments
- The length of MAC in centimeters
Only MAC identified through the segmentation method was able to independently predict whether a patient would also experience peripheral artery disease and diabetic nephropathy, the authors noted. However, both methods for calculating MAC from ultrasound scans were still valuable.
"Consistent with previous studies, the presence and severity of MAC were associated with diabetic complications in our univariate analysis, regardless of whether the length or segmentation method was used," wrote the authors, led by Jing Tian from Sun Yat-Sen Memorial Hospital in Guangzhou, China.
Ultrasound is one tool that can be used to help screen patients with diabetes for MAC, but there is no consensus on the best scoring method to evaluate MAC severity from ultrasound scans. Therefore, the authors compared two commonly used scoring systems: the segmentation method and the length method.
In the length method, MAC severity is determined based on the severity of calcification in a 4-cm scanned area. A MAC length of 0 cm, less than 1 cm, 1 to 2 cm, 2 to 3 cm, and greater than 3 cm on ultrasound scans correspond to MAC scores of 0, 1, 2, 3, and 4, respectively. The scores are then added up, with higher scores indicating higher MAC severity.
In the segmentation method, a point is given for the presence of any MAC in the superficial femoral artery to popliteal artery segment, the anterior tibial artery to dorsalis pedis artery segment, and the posterior tibial artery and peroneal artery segment. Like in the length method, the scores are added up, and higher scores indicate higher MAC severity.
The researchers used both MAC scoring methods on 359 patients with type 2 diabetes who stayed at a hospital endocrinology department between March 2015 and December 2017. A radiologist with 15 years of clinical ultrasound experience performed the bilateral lower limb artery ultrasound examinations on the patients.
About 37% of patients had MAC based on the ultrasound scan findings, but the diagnosis of mild and severe MAC differed based on the scoring approach. Using the length method, the researchers found 105 mild MAC cases and 123 severe cases, whereas the segmentation method identified 98 mild cases and 130 severe ones.
Both methods helped predict the odds of diabetic complications, including peripheral artery disease, peripheral neuropathy, retinopathy, and nephropathy. However, the segmentation method was also an independent predictor of peripheral artery disease and diabetic nephropathy, suggesting it may be better for evaluating cardiovascular abnormalities and risk for diabetes complications.
A main limitation of the study was that it only included ultrasound imaging instead of also using another imaging modality, the authors noted. However, it also demonstrated that two different ultrasound scoring methods can help predict diabetic complications -- although the segmentation might be better.
"MAC scores calculated by the segmentation method were significantly correlated with [peripheral arterial disease] and diabetic nephropathy," they concluded. "The segmentation method for assessing MAC may be a valuable tool in clinical work."
Đăng ký:
Nhận xét
(
Atom
)




