Tổng số lượt xem trang
Thứ Ba, 1 tháng 9, 2020
Blood pressure monitor trades compression for US
By Theresa Pablos, AuntMinnie staff writer
September 1, 2020 -- Researchers from Japan have developed a blood pressure monitor that utilizes a tiny ultrasound probe instead of compression to monitor systolic and diastolic changes. The science behind the prototype was presented as a virtual poster at the 2020 European Society of Cardiology (ESC) Conference. Lead author Dr. Kazunori Uemura, PhD, and his team from the National Cerebral and Cardiovascular Center in Japan designed the ultrasound-based monitor to unobtrusively track blood pressure on-the-go. Once calibrated, the ultrasound-based device produced blood pressure readings comparable to conventional technology in dogs.
"This method reliably tracks [blood pressure] changes without occlusive cuff inflation," the authors wrote in their poster abstract.
Monitoring blood pressure out-of-the-office and at regular intervals is important for hypertension diagnosis and management, but current compression-based blood pressure monitors can interfere with the daily lives of patients. Uemura and colleagues saw ultrasound as a potential alternative to compression-based technology.
The cuff they created utilizes a tiny ultrasound probe about half the size of a box of matches. The probe sits snugly in between a patient's skin and the larger blood pressure cuff.
Upon mild cuff inflation, the ultrasound transducer's 65 piezoelectric elements measure changes to an artery situated underneath the probe. Uemura and colleagues use these measurements to calculate estimated diastolic and systolic blood pressure.
(A) Schematic illustration of the cuff and ultrasound probe wrapped around the upper arm and positioned over the brachial artery. (B) Longitudinal cross section illustration of the ultrasound probe and inflated cuff. When the cuff is inflated, the device tracks the ultrasonic dimension of the brachial artery. Image courtesy of Dr. Kazunori Uemura, PhD.
The authors tested the cuff's accuracy for blood pressure monitoring on the right femoral artery of six anesthetized dogs. Measurements taken with the ultrasound-based device correlated strongly with compression-based readings, according to coefficient of determination (R2) analysis.
With just one-time calibration, the diastolic blood pressure readings had a bias of 3.9 ± 7.9 mmHg. This measurement fell within the acceptable bias range of < 5 ± < 8 mmHg set by the Association for the Advancement of Medical Instrumentation (AAMI).
However, with one-time calibration, the systolic blood pressure readings had a bias of 2.6 ± 18.9 mmHg, outside of the AAMI acceptable range. To improve the systolic readings, the authors added machine learning and a support vector algorithm to the initial, one-time calibration. The new analysis yielded systolic measurements with a bias of 0.7 ± 6.9 mmHg, meeting the AAMI guidelines.
"Once calibrated, this method measures [diastolic blood pressure] accurately," the authors wrote. "With the aid of machine learning, precision in [systolic blood pressure] prediction was greatly improved to acceptable levels."
This type of ultrasound-based technology is a long way from use in the clinic, and the research team still has yet to test the device's accuracy on people. But if the cuff holds up in further testing, the combination of ultrasound and machine learning could lead to better mobile blood pressure monitoring.
"This method with machine learning approach has potential for stress-free [blood pressure] measurement in ambulatory [blood pressure] monitoring," the authors concluded.
Thứ Ba, 25 tháng 8, 2020
Carotid lumen size linked to death from all causes
By Theresa Pablos, AuntMinnie staff writer
August 21, 2020 -- Could ultrasound measurements of the carotid lumen diameter be a better measure than carotid intima-media thickness (CIMT) for predicting mortality from cardiovascular disease? Lumen diameter indeed could add new information, according to a study in the Journal of the American Heart Association.
Researchers from Germany found that lumen diameter measurements of the carotid artery derived from ultrasound scans predicted mortality from both cardiovascular disease and from all causes. And they believe that it provides more information than CIMT.
CIMT has been used as a noninvasive biomarker for cardiovascular disease risk stratification and the risk of future cardiovascular events, the authors report. Both the coronary and carotid arteries distend during the early stages of atherosclerosis, a phenomenon that can be detected and measured on ultrasound scans.
But recent research has raised doubts about the reliability of CIMT for predicting individual outcomes. The new evidence, published on August 4, demonstrates that lumen size might be a better predictor of death from both cardiovascular and noncardiovascular events, with larger lumens indicating higher risk.
"Our results suggest that [lumen diameter] may be superior to CIMT," wrote the authors, led by Dr. Felix Fritze from the University of Greifswald's medical school in Greifswald, Germany.
The team of German researchers compared the effectiveness of CIMT and lumen diameter using data from a prior study that conducted baseline screenings and 10- and 15-year follow-up exams on the population of a German village.
As part of the baseline assessment, individuals underwent carotid ultrasonography. The original research team also recorded relevant health information, including cholesterol levels, diabetes status, and mortality outcomes.
For the new analysis, Fritze and colleagues created various models to analyze data from 2,751 participants, including 506 who died during the original study. Their further cardiovascular mortality analysis used outcomes from all but 214 of the participants with unknown causes of death.
The researchers found that individuals with the largest CIMT measurements had the highest hazard ratio (HR) for all-cause mortality, at 1.73, compared with a hazard ratio for lumen diameter of 1.29 and the combination of CIMT and lumen diameter at 1.26.
The model using lumen diameter alone was significantly associated with death from all causes, deaths attributed to cardiovascular events, and deaths attributed to noncardiovascular events. On the other hand, the model using CIMT alone was significantly associated with all-cause mortality and noncardiovascular mortality -- but not cardiovascular mortality.
To help determine the likelihood of their models predicting future values, the authors conducted an Akaike information criterion (AIC) analysis. In this analysis, the lumen diameter model came out on top for both all-cause mortality and cardiovascular mortality. It also came in second for cardiovascular mortality, just behind a model that combined lumen size and CIMT values.
Furthermore, the lumen diameter model remained significant for all-cause mortality even after the researchers excluded people with chronic kidney disease, prior myocardial infarction, and type 2 diabetes. The same wasn't true for the CIMT model.
| Lumen diameter vs. CIMT for predicting mortality | |||
| Model | Rank (AIC) | ||
| All-cause mortality | Cardiovascular mortality | Noncardiovascular mortality | |
| Lumen diameter | No. 1 | No. 1 | No. 2 |
| Lumen diameter + CIMT | No. 2 | No. 2 | No. 1 |
| CIMT | No. 3 | No. 5 | No. 3 |
| None | No. 4 | No. 4 | No. 4 |
| Lumen diameter ÷ CIMT | No. 5 | No. 3 | No. 5 |
The authors do not know why the model using lumen diameter performed much better than CIMT in their analysis. They hypothesized it could be because lumen size is related to CIMT but is also much easier to measure.
"The larger caliber of [lumen diameter] compared with CIMT may improve manual measurement accuracy and thus may be more applicable for an outpatient setting," they wrote.
It's important to note the study only included white participants from one part of Germany, so the results may not be applicable to a more diverse population. As a result, the authors called for follow-up research with more robust patient populations to verify their findings.
"To the best of our knowledge, this is the first study to compare the informative value of CIMT and [lumen diameter] with regard to all-cause, cardiovascular, and noncardiovascular mortality associations," they concluded. "We report that [lumen diameter] provides more information than CIMT."
Thứ Hai, 24 tháng 8, 2020
US effective for working up masses found on DBT
By Kate Madden Yee, AuntMinnie.com staff writer
August 24, 2020 -- Ultrasound appears to be an effective and safe diagnostic workup modality when it comes to evaluating masses identified on screening digital breast tomosynthesis (DBT), according to research published in the European Journal of Radiology (EJR).
The findings suggest that, at least in the case of breast masses, it may not be necessary for women to undergo both digital mammography and ultrasound after screening DBT -- which has the benefit of reducing radiation exposure, wrote a group led by Dr. Jessica Porembka of the University of Texas Southwestern Medical Center in Dallas.
"DBT has been shown to be superior to conventional views in the diagnostic setting ... [and] women who already underwent screening DBT may be receiving unnecessary digital mammography prior to ultrasound imaging," the group wrote in an EJR article posted on August 5. "This potentially adds unnecessary complexity, cost, and radiation exposure, as well as prolonged diagnostic workup times without adding significant value."
Screening DBT reduces recalls compared with digital mammography alone, but still, sometimes follow-up is needed. Porembka and colleagues investigated whether in some of these cases --perhaps by type of lesion found on DBT -- women could undergo ultrasound alone rather than also having additional mammography.
The study included 266 noncalcified lesions in 247 women detected on screening DBT between January 2014 and December 2016. The lesions ranged from architectural distortions and asymmetries to focal asymmetries and masses. The investigators assessed the number and type of lesions that underwent diagnostic follow-up only with ultrasound.
The researchers found that ultrasound alone was used in 69% of workups of recalled masses, and that the odds of masses being worked up with ultrasound alone was eight times that of the odds of digital mammography and ultrasound being used. The authors also found that "ultrasound alone in the diagnostic evaluation of a mass seen on screening DBT had a higher yield of true lesions than masses worked up with digital mammography/ultrasound," confirming that "masses seen on screening DBT can be adequately evaluated with ultrasound alone."
However, ultrasound alone did less well with architectural distortions and focal asymmetries, with a detection rate of 44% and 25%, respectively, Porembka and colleagues cautioned.
"Our findings suggest that a combination of both [digital mammography and ultrasound] was preferred by radiologists in the work up of architectural distortions given the differential diagnosis of radial scar versus malignancy," the team noted. "For focal asymmetries, 68% were evaluated with digital mammography/ultrasound, while only 25% were evaluated with ultrasound alone, indicating that a combination of digital mammography/ultrasound is likely warranted in the work up of focal asymmetry on DBT."
In any case, the study results are good news for women undergoing diagnostic follow-up for masses found on screening DBT, according to the researchers.
"The implication of our findings is that we can save women unnecessary radiation and unnecessary cost of digital mammography by utilizing ultrasound alone in the evaluation of recalled masses," they concluded.
Thứ Sáu, 21 tháng 8, 2020
Transcranial U S helps solve COVID-19 mystery
By Theresa Pablos, AuntMinnie staff writer
August 21, 2020 -- Ultrasound scans with a robotic transcranial Doppler device provided a clue into why patients with COVID-19 experience severe hypoxemia without lung stiffness. In a serendipitous discovery, researchers linked the ultrasound findings to suspiciously low oxygen levels in patients with severe cases of COVID-19.
The researchers used a robotic transcranial Doppler (TCD) ultrasound system to assess cerebral blood flow in 18 patients with severe COVID-19 pneumonia. They had been looking for stroke and other cranial abnormalities, but they instead found that the majority of patients had detectable microbubbles, a finding that indicates abnormally dilated pulmonary blood vessels.
"This study helps explain the strange phenomenon seen in some COVID-19 patients known as 'happy hypoxia,' where oxygen levels are very low, but the patients do not appear to be in respiratory distress," stated senior author Dr. Hooman Poor, an assistant professor at the Icahn School of Medicine at Mount Sinai in a press release. Poor and colleagues published their research on August 6 as a letter in the American Journal of Respiratory and Critical Care Medicine.
In patients with classic acute respiratory distress syndrome (ARDS), pulmonary inflammation results in blood vessel changes that make the lungs stiff and impair oxygenation. But the amount of hypoxemia seen in patients with COVID-19 is often drastically out of proportion with lung stiffness.
The new pilot study revealed that vasodilation could help explain why COVID-19 pneumonia differs from classic ARDS. Using transcranial Doppler ultrasound scans, the researchers found that 83% of patients had detectable microbubbles. In addition, the number of microbubbles correlated with hypoxemia severity in patients with severe COVID-19.
In comparison, only about 26% of patients with classic ARDS show detectable microbubbles on transcranial Doppler scans. The number of microbubbles also did not correlate with hypoxemia severity for patients with classic ARDS.
"It is becoming more evident that the virus wreaks havoc on the pulmonary vasculature in a variety of ways," stated Poor.
The study included 18 patients with severe COVID-19 pneumonia who also had altered mental status and required mechanical ventilation. The patients underwent robotic transcranial Doppler ultrasound (Lucid Robotic System by NovaSignal) with an agitated saline solution.
The researchers injected the contrast agent in an upper extremity or through a central line in the internal jugular vein. NovaSignal's ultrasound software automatically counted the number of microbubbles detected over 20 seconds, and the researchers manually counted and confirmed the number of microbubbles as a precaution.
In healthy patients, the contrast microbubbles enter the lung blood vessels and get filtered out by pulmonary capillaries. If bubbles are detected in the brain, it indicates that the patient either has a hole in the heart or that the capillaries are abnormally dilated, which the researchers believe might be contributing to hypoxemia in patients with COVID-19.
Poor and his team at Mount Sinai are continuing their research and have thus far collected data from roughly 80 patients with various COVID-19 severity. The team plans to analyze microbubble transit, including how transit varies throughout the course of the disease.
"If these findings are confirmed in larger studies, pulmonary microbubble transit may potentially serve as a marker of disease severity or even a surrogate endpoint in therapeutic trials for COVID-19 pneumonia," Poor stated. "Future studies that investigate the use of pulmonary vascular constrictors in this patient population may be warranted."
Thứ Tư, 19 tháng 8, 2020
Doppler U S helps assess cervical cancer stage
By Theresa Pablos, AuntMinnie staff writer
August 18, 2020 -- Researchers in China found a link between findings on Doppler ultrasound scans and characteristics of cervical cancer. Blood flow seen through color ultrasound was tied to tumor clinical stage, cancer type, and pathology in a study published on August 10 in PLOS One.
Imaging to assist with cancer staging is crucial, and there have been calls to include more radiological imaging in cervical cancer diagnosis and staging. The new findings suggest Adler grades -- a scoring system that reflects tumor vascularization -- may help physicians assess cervical cancers using color ultrasound.
"Adler grades are closely associated with the clinical pathology of cervical cancer, which may be a convenient and effective approach for the assisting assessment of cervical cancer," wrote the authors, led by Dr. Dehong Che from the department of obstetrics and gynecology at the Second Affiliated Hospital of Harbin Medical University in Harbin, China.
Prior research found that color Doppler ultrasound scans may accurately determine tumor size, invasiveness, and vascular patterns. But while Doppler ultrasound is used in the assessment of other cancers, it is not as common for gynecological cancer assessment, the authors noted.
To determine the effectiveness of Doppler ultrasound on cervical cancer assessment, the authors enrolled 162 patients in their study. The patients had pathologically confirmed cervical cancer cases and no prior history of malignancy, cervical surgery, or uterine malformations.
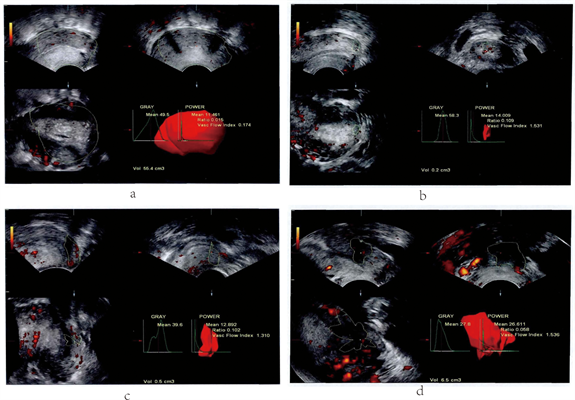
A sonographer first performed a grayscale sonography examination to evaluate the cervical area and surrounding tissue before studying blood flow with Doppler ultrasound. A radiologist and a gynecologist determined an Adler grade for the tumor based on the blood flow to the lesion.
| Adler score and ultrasound findings on cervical cancer tumors | ||
| Adler score | Definition | Ultrasound findings |
| Grade 0 | No obvious blood flow | • Normal appearance |
| Grade 1 | 1-2 blood vessels with a diameter of < 1 mm | • Slightly thickened morphology
• More enhanced intra-cervical echo
• Spot-like blood flow signals
|
| Grade 2 | 3-4 blood vessels with a diameter of < 1 mm | • Uneven or thickened cervical echo
• Strip blood flow
|
| Grade 3 | More than 4 blood vessels or vessels are intertwined into a network | • Parauterine and extrauterine invasion
• Reticular blood flow
|
Click image to enlarge.
Doppler ultrasound images of cervical cancers with different Adler scores: (A) Grade 0, (B) Grade 1, (C) Grade 2, and (D) Grade 3. Images courtesy of Che D, Yang Z, Wei H, Wang X, Gao J (2020) The Adler grade by Doppler ultrasound is associated with clinical pathology of cervical cancer: Implication for clinical management. PLOS ONE, 15(8): e0236725. https://doi.org/10.1371/journal.pone.0236725.
Patients with a higher Adler score had higher clinical stages of cervical cancer, the authors found. Adler score was significantly associated with the International Federation of Gynecology and Obstetrics (FIGO) clinical stage, pathological tumor type, and squamous cell carcinoma subtypes.
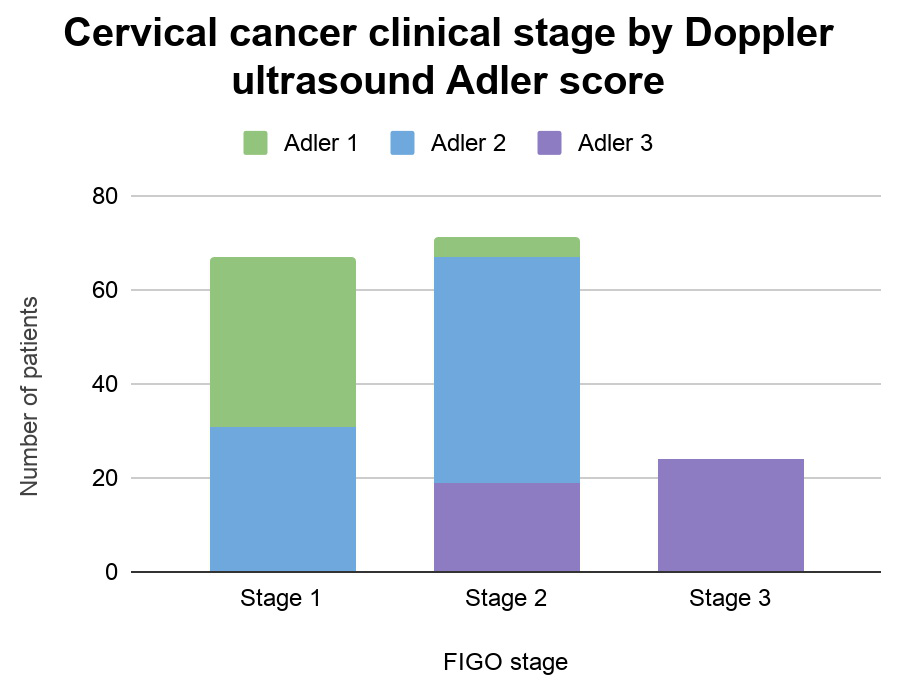
Compared with FIGO stages, Adler grade achieved an area under the curve (AUC) of 0.811, with a sensitivity of 55% and specificity 90%. Compared with pathological stage results, Adler grade achieved an AUC of 0.76, with a sensitivity of 52% and specificity of 88%.
"Those results indicated that Adler grade could provide valuable reference for the diagnosis of cervical cancer," the authors wrote.
Cervical cancer is known for its rapid proliferation and active cell division -- two characteristics related to blood vessel proliferation. As a result, this type of cancer may translate particularly well to Doppler imaging, the authors noted.
"On color Doppler ultrasound images, there are often abundant different types of blood flow signals in tumor tissues, which correspond to its rich vascular network and are related to the special structure and blood flow characteristics of tumor blood vessels," they wrote.
The authors cautioned their study had a small sample size and that subjective factors can influence the Adler score. Nevertheless, they concluded that the use of Doppler ultrasound should be considered when working with patients with suspected or newly diagnosed cervical cancer.
"With the continuous development of ultrasound technology and population of clinical ultrasound applications, Adler grade should be promoted in the application of color Doppler ultrasound for the diagnosis and treatment of cervical cancer," the authors wrote.
Đăng ký:
Nhận xét
(
Atom
)
