By Theresa Pablos, AuntMinnie staff writer
September 25, 2020 -- A pocket-sized ultrasound scanner powered by a smartphone performed comparably to a cart-based scanner for lung imaging at the point of care in patients with COVID-19, according to a study published on September 21 in Ultrasound in Medicine and Biology.
In the head-to-head study, a team of Italian authors compared a conventional, portable cart-based ultrasound scanner with a pocket-sized device for point-of-care ultrasound (POCUS) of COVID-19 patients. The smaller -- and cheaper -- system adequately visualized pulmonary regions of patients with COVID-19.
The findings are good news in a pandemic rife with medical equipment shortages.
"Our study confirms the possibilities of portable pocket-sized ultrasound imaging of the lung in COVID-19 patients," wrote the authors, led by Dr. David Bennett from the University Hospital of Siena in Siena, Italy.
Lung ultrasound has repeatedly proved its usefulness as a tool to diagnose and monitor patients with COVID-19. While prior studies on the topic have used portable ultrasound systems, no research has directly compared the performance of pocket-sized ultrasound systems with larger scanners for COVID-19 imaging.
In the latest study, clinicians performed lung ultrasound scans on 18 patients hospitalized with COVID-19 at the University Hospital of Siena. The patients were all symptomatic, tested positive for SARS-CoV-2, and had radiologic evidence of interstitial pneumonia.
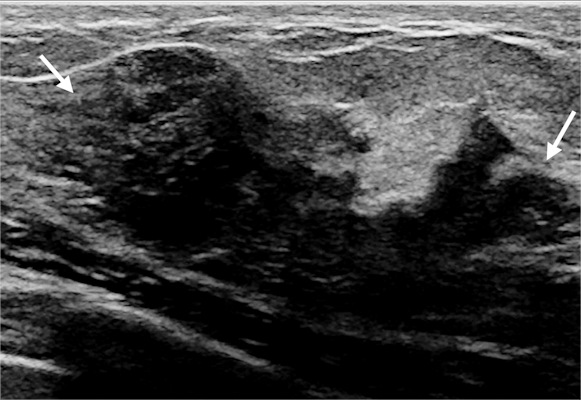
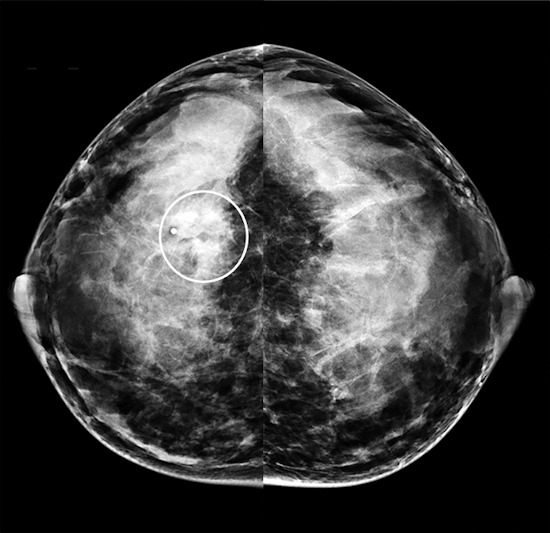
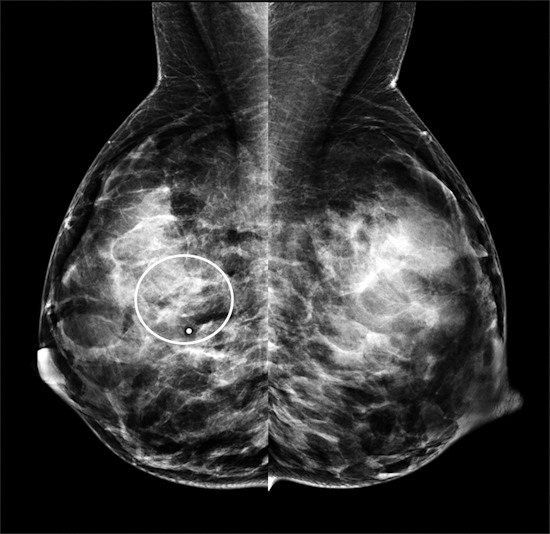
Clinicians scanned the patients using two ultrasound systems: (1) Venue Go by GE Healthcare, a cart-based system with built-in artificial intelligence capabilities, and (2) Butterfly iQ by Butterfly Network, a pocket-sized system powered by a smartphone that uses a silicon chip instead of a piezoelectric crystal.
The team used the scans to calculate patients' lung ultrasound scores, a proven method for quantifying pulmonary disease severity in patients with COVID-19. The scoring system works by assigning numerical scores of 0-3 to unique lung regions. Higher scores indicate worse disease severity.
The team found no significant difference between the two systems for patients' overall lung ultrasound scores. Lung scores obtained by both systems also correlated with patients' clinical severity.
In addition, the scores were comparable for most individual pulmonary regions, including the left and right side and vertical location. However, the team did find an 0.082 score difference between the systems for horizontal position, a statistically significant finding they deemed a "practically negligible difference in the posterior side of the thorax."
Further statistical analysis revealed a bias of -0.016 between the systems with very narrow limits of agreement.
"The results of the portable scanner were practically identical to the high-end scanner in the assessment of lung interstitial syndrome," the authors wrote.
While pocket-sized scanners are easy to carry and significantly cheaper than larger models, they also come with a number of drawbacks. Small systems tend to have limited battery life, reduced field of vision, and low penetration, the authors noted.
The authors also cautioned that POCUS should be used with clinical and physiological data for patients with COVID-19. However, they were also confident that pocket-sized systems could accurately assess lung lesions -- and do so more affordably than high-end scanners.
"These ultrasound scanners can play a decisive role when healthcare resources are scarce, during pandemics and in emergency situations, such as the present COVID-19 outbreak," the authors concluded.