Tổng số lượt xem trang
Thứ Sáu, 29 tháng 6, 2018
SIÊU ÂM ĐẦU CỔ TRONG CẤP CỨU.
https://blogger.googleusercontent.com/img/proxy/AVvXsEjEduRQAhudhXHqKDYVQM9GkKG8du-cSsx2Podlc_2xyk6TMQY04PyqrKfYl44ucJJdYZVLM_soxA57oSsQHPiXzDQ-vlZcLbU-m8P-IF_5j0shlDIc9yACP3F7g45NpnA3l-DTLwDmB8AZ2XmXwpC7IcLBkwrRkg5oGRBc16IQNOFLSRrz0fXP412d=s0-d-e1-ft
Thứ Năm, 28 tháng 6, 2018
SIÊU ÂM ĐÀN HỒI và GAN HOÁ XƠ Ở TRẺ NẶNG CÂN
Nonalcoholic fatty liver disease is the most common chronic liver disease in overweight adolescents. In most cases, the disease will remain stable for decades without causing significant impairment of liver function. If the disease progresses, persistent inflammation in the liver will cause the formation of excess connective tissue - a stage known as liver fibrosis. Eventually, the disease may damage the liver's entire cellular structure, resulting in what is known as 'liver cirrhosis'.
"Time-harmonic elastography is a new, ultrasound-based technology used to measure liver fibrosis. It works without the need for invasive liver biopsies," explains Dr. Christian Hudert, a pediatric gastroenterologist from Charité's Center for chronically sick children (SPZ). Until now, the grading and staging of liver disease has only been possible through the analysis of tissues taken at biopsy. Elastography is capable of visualizing differences in the elasticity of different tissues. In patients with liver fibrosis, excess connective tissue causes the liver to be stiffer than a normal liver and means that liver stiffness constitutes a measure of disease progression.
The trolley on which the patient is positioned during their examination is a special and defining characteristic of Charité's THE technology. This trolley produces vibrational waves, which are not unlike those produced by a massage chair. Using ultrasound technology, these waves are then measured inside the liver tissue, thus providing information on liver stiffness. In contrast to previous elastography techniques, this technology is capable of taking measurements at greater tissue depths, making it particularly suitable for use in obese patients.
This study used the newly-developed technology to examine 67 adolescents with nonalcoholic fatty liver disease. Liver stiffness measurements were used to determine the degree of fibrosis present. Summing up the study's findings, Dr. Hudert explains: "The THE technology was shown to be capable of accurately distinguishing between patients with no fibrosis or mild fibrosis and patients with moderate or advanced fibrosis." Should the technology prove successful in further studies, it may eventually reduce the need for patients to undergo invasive liver biopsies. The THE method is also particularly suitable for use in the long-term monitoring of patients and may help to verify the success of weight loss treatment options as well as their impact on the outcome of liver disease.
Thứ Tư, 27 tháng 6, 2018
Appendicitis and Clinical Ultrasound
Appendicitis and CUS
Abstract
Introduction: Clinical ultrasound (CUS) is highly specific for the diagnosis of acute appendicitis but is operator-dependent. The goal of this study was to determine if a heterogeneous group of emergency physicians (EP) could diagnose acute appendicitis on CUS in patients with a moderate to high pre-test probability.
Methods: This was a prospective, observational study of a convenience sample of adult and pediatric patients with suspected appendicitis. Sonographers received a structured, 20-minute CUS training on appendicitis prior to patient enrollment. The presence of a dilated (>6 mm diameter), non-compressible, blind-ending tubular structure was considered a positive study. Non-visualization or indeterminate studies were considered negative. We collected pre-test probability of acute appendicitis based on a 10-point visual analog scale (moderate to high was defined as >3), and confidence in CUS interpretation. The primary objective was measured by comparing CUS findings to surgical pathology and one week follow-up.
Results: We enrolled 105 patients; 76 had moderate to high pre-test probability. Of these, 24 were children. The rate of appendicitis was 36.8% in those with moderate to high pre-test probability. CUS were recorded by 33 different EPs. The sensitivity, specificity, and positive and negative likelihood ratios of EP-performed CUS in patients with moderate to high pre-test probability were 42.8% (95% confidence interval [CI] [25-62.5%]), 97.9% (95% CI [87.5–99.8%]), 20.7 (95% CI [2.8–149.9]) and 0.58 (95% CI [0.42–0.8]), respectively. The 16 false negative scans were all interpreted as indeterminate. There was one false positive CUS diagnosis; however, the sonographer reported low confidence of 2/10.
Conclusion: A heterogeneous group of EP sonographers can safely identify acute appendicitis with high specificity in patients with moderate to high pre-test probability. This data adds support for surgical consultation without further imaging beyond CUS in the appropriate clinical setting.
Thứ Hai, 25 tháng 6, 2018
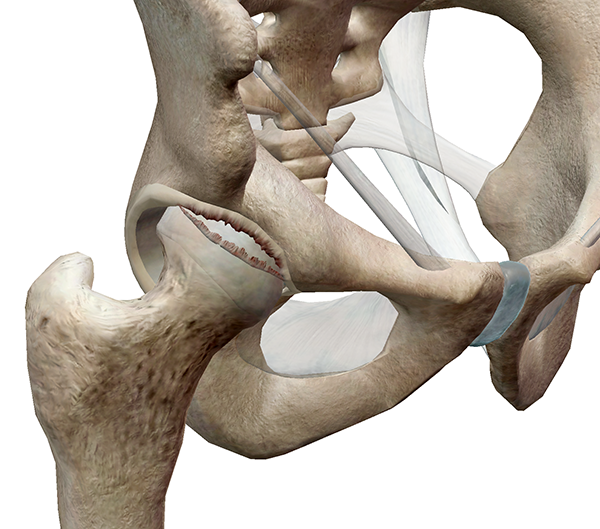
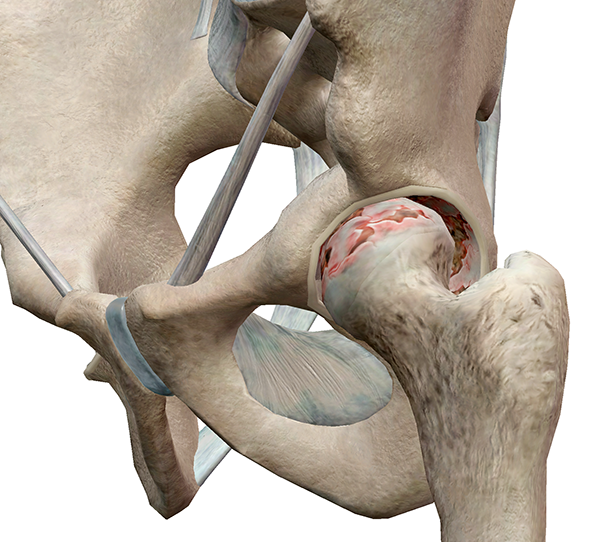
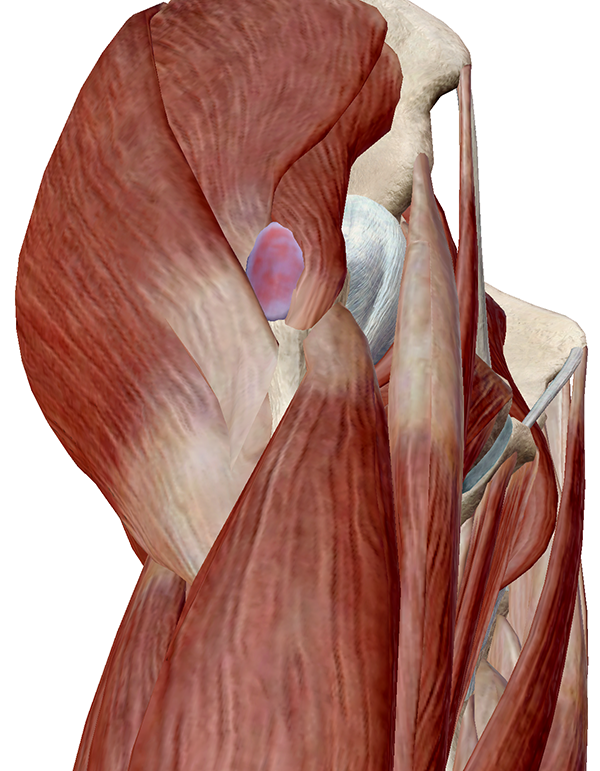
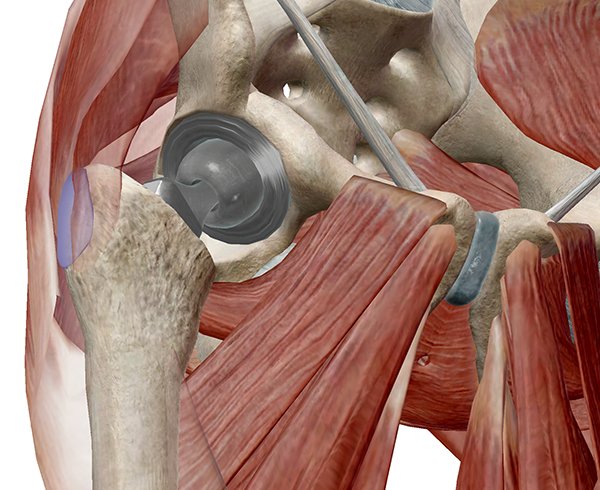
Four Common Pathologies of the Hip Region
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Thứ Sáu, 22 tháng 6, 2018
I B D in Children and Ultrasound
Abstract
Background
Magnetic resonance enterography (MRE) is the current gold standard for imaging in inflammatory bowel disease, but ultrasound (US) is a potential alternative.
Objective
To determine whether US is as good as MRE for the detecting inflamed bowel, using a combined consensus score as the reference standard.
Materials and methods
We conducted a retrospective cohort study in children and adolescents under 18 years with inflammatory bowel disease (IBD) at a tertiary and quaternary centre. We included children who underwent MRE and US within 4 weeks. We scored MRE using the London score and US using a score adapted from the METRIC (MR Enterography or Ultrasound in Crohn’s Disease) trial. Four gastroenterologists assessed an independent clinical consensus score. A combined consensus score using the imaging and clinical scores was agreed upon and used as the reference standard to compare MRE with US.
Results
We included 53 children. At a whole-patient level, MRE scores were 2% higher than US scores. We used Lin coefficient to assess inter-observer variability. The repeatability of MRE scores was poor (Lin 0.6). Agreement for US scoring was substantial (Lin 0.95). There was a significant positive correlation between MRE and clinical consensus scores (Spearman’s rho = 0.598, P=0.0053) and US and clinical consensus scores (Spearman’s rho = 0.657, P=0.0016).
Conclusion
US detects as much clinically significant bowel disease as MRE. It is possible that MRE overestimates the presence of disease when using a scoring system. This study demonstrates the feasibility of using a clinical consensus reference standard in paediatric IBD imaging studies.
Keywords
Adolescents Children Diagnostic accuracy Inflammatory bowel disease Magnetic resonance imaging Reproducibility UltrasoundThứ Năm, 21 tháng 6, 2018
Elastography of the GI Tract.
Odd Helge Gilja, Prof., MD, PhD National Centre for Ultrasound in Gastroenterology Haukeland University Hospital, Bergen, and Department of Clinical Medicine, University of Bergen, Norway.
Elastography is a relative new technique that depicts the stiffness of tissue and is already used in clinical practice for several indications.
Guidelines and recommendations of the different techniques and clinical applications was published by EFSUMB. Elastography and strain imaging has also been suggested as a tool for assessing diseases of the gastrointestinal tract.
The bowel wall is a thin structure, which does not make it the ideal organ to be studied with elastography. However, pathology of the GI tract such as inflammation or tumour causes bowel wall thickening and often reduces motility and luminal contents in the affected area which may facilitate strain imaging. There is evidence for the use of elastography in endorectal ultrasonography, but the evidence for transabdominal elastography of the bowel is sparse. However, some recent studies suggest that it can be used to differentiate between fibrotic and inflammatory stenosis in Crohn’s disease. In patients with a stricture of the bowel and resultant bowel obstruction, it is important to determine if there is active inflammation at the site of stricture or if the obstructed segment is fibrotic. Using elastography, the active inflammatory components will be softer whereas the fibrotic stricture will appear stiffer. Accordingly, one may apply elastography to evaluate stiffness of the stenotic area, thus providing more clues to the fibrous content of the stricture. In conclusion, elastography may become a relevant clinical tool, but we need more studies to determine its usefulness in the management of patients with GI diseases.
References: 1. Bamber J, Cosgrove D, Dietrich CF, Fromageau J, Bojunga J, Calliada F, Cantisani V, Correas JM, D’Onofrio M, Drakonaki EE, Fink M, Friedrich-Rust M, Gilja OH,Havre RF,JenssenC,KlauserAS,Ohlinger R, Saftoiu A,SchaeferF, SporeaI,PiscagliaF. EFSUMBGuidelinesand Recommendations on the Clinical Use of Ultrasound Elastography. Part 1: Basic Principles and Technology. Ultraschall Med. 2013 Apr;34(2):169-84. http://dx.doi.org/10.1055/s-00331335205. Epub 2013 Apr 4. 2. Cosgrove D, Piscaglia F, Bamber J, Bojunga J, Correas JM, Gilja OH, Klauser AS, Sporea I, Calliada F, Cantisani V, D’Onofrio M, Drakonaki EE, Fink M, Friedrich-Rust M, Fromageau J, Havre RF, Jenssen C, Ohlinger R, Saftoiu A, Schaefer F, Dietrich CF. EFSUMBGuidelines and Recommendations on the Clinical Use of Ultrasound Elastography.
Elastography is a relative new technique that depicts the stiffness of tissue and is already used in clinical practice for several indications.
Guidelines and recommendations of the different techniques and clinical applications was published by EFSUMB. Elastography and strain imaging has also been suggested as a tool for assessing diseases of the gastrointestinal tract.
The bowel wall is a thin structure, which does not make it the ideal organ to be studied with elastography. However, pathology of the GI tract such as inflammation or tumour causes bowel wall thickening and often reduces motility and luminal contents in the affected area which may facilitate strain imaging. There is evidence for the use of elastography in endorectal ultrasonography, but the evidence for transabdominal elastography of the bowel is sparse. However, some recent studies suggest that it can be used to differentiate between fibrotic and inflammatory stenosis in Crohn’s disease. In patients with a stricture of the bowel and resultant bowel obstruction, it is important to determine if there is active inflammation at the site of stricture or if the obstructed segment is fibrotic. Using elastography, the active inflammatory components will be softer whereas the fibrotic stricture will appear stiffer. Accordingly, one may apply elastography to evaluate stiffness of the stenotic area, thus providing more clues to the fibrous content of the stricture. In conclusion, elastography may become a relevant clinical tool, but we need more studies to determine its usefulness in the management of patients with GI diseases.
References: 1. Bamber J, Cosgrove D, Dietrich CF, Fromageau J, Bojunga J, Calliada F, Cantisani V, Correas JM, D’Onofrio M, Drakonaki EE, Fink M, Friedrich-Rust M, Gilja OH,Havre RF,JenssenC,KlauserAS,Ohlinger R, Saftoiu A,SchaeferF, SporeaI,PiscagliaF. EFSUMBGuidelinesand Recommendations on the Clinical Use of Ultrasound Elastography. Part 1: Basic Principles and Technology. Ultraschall Med. 2013 Apr;34(2):169-84. http://dx.doi.org/10.1055/s-00331335205. Epub 2013 Apr 4. 2. Cosgrove D, Piscaglia F, Bamber J, Bojunga J, Correas JM, Gilja OH, Klauser AS, Sporea I, Calliada F, Cantisani V, D’Onofrio M, Drakonaki EE, Fink M, Friedrich-Rust M, Fromageau J, Havre RF, Jenssen C, Ohlinger R, Saftoiu A, Schaefer F, Dietrich CF. EFSUMBGuidelines and Recommendations on the Clinical Use of Ultrasound Elastography.
Đăng ký:
Bài đăng
(
Atom
)