By Theresa Pablos, AuntMinnie staff writer
March 19, 2020 -- Ultrasound scans show promise for helping to monitor patients with COVID-19, according to a letter published on March 12 in Intensive Care Medicine. The researchers used lung ultrasonography to monitor more than a dozen patients in China with COVID-19 infections.
Because of its high sensitivity, CT is currently the imaging method of choice to diagnose and monitor patients with COVID-19. However, chest CT may also present difficulties for patients with hypoxemia and hemodynamic failure, and the enclosed environment may contribute to the spread of the coronavirus.
In the research letter, the authors found lung ultrasonography could overcome some of CT's limitations. Ultrasound may even be the better imaging choice for patients in critical condition who cannot be easily moved.
"Based upon our experience, we consider that lung ultrasonography has major utility for management of COVID-19 with respiratory involvement due to its safety, repeatability, absence of radiation, low cost, and point of care use," wrote the authors, led by Qian-Yi Peng, from the critical care department at Xiangya Hospital in Changsha, China.
COVID-19 on lung ultrasound scans
Peng and colleagues performed lung ultrasonography on 20 patients with COVID-19. They used a 12-zone examination method, which resulted in the following five characteristic findings:
- Pleural line thickening and irregularity
- Variety of B-line patterns, including focal, multifocal, and confluent
- Variety of consolidation patterns, including multifocal small, nontranslobar, and translobar with occasional mobile air bronchograms
- Visible A-lines during the recovery phase
- Rare occurrence of pleural effusions
"The observed patterns occurred across a continuum from mild alveolar interstitial pattern, to severe bilateral interstitial pattern, to lung consolidation," the authors wrote.
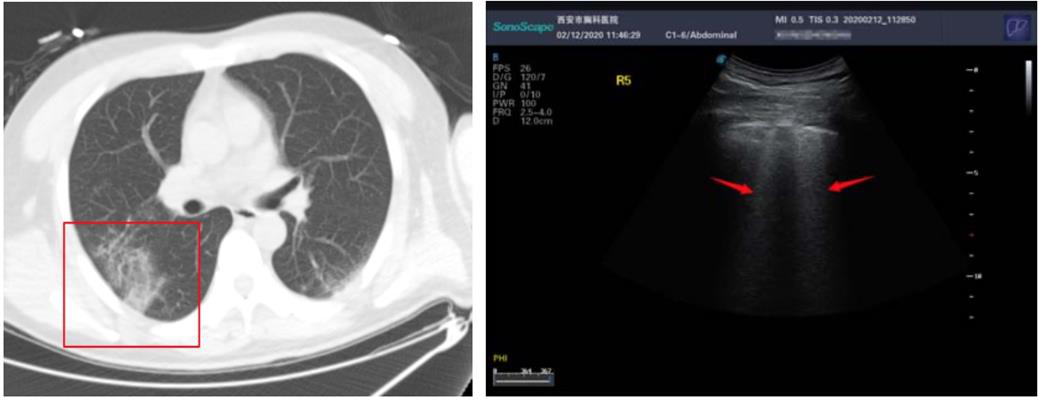
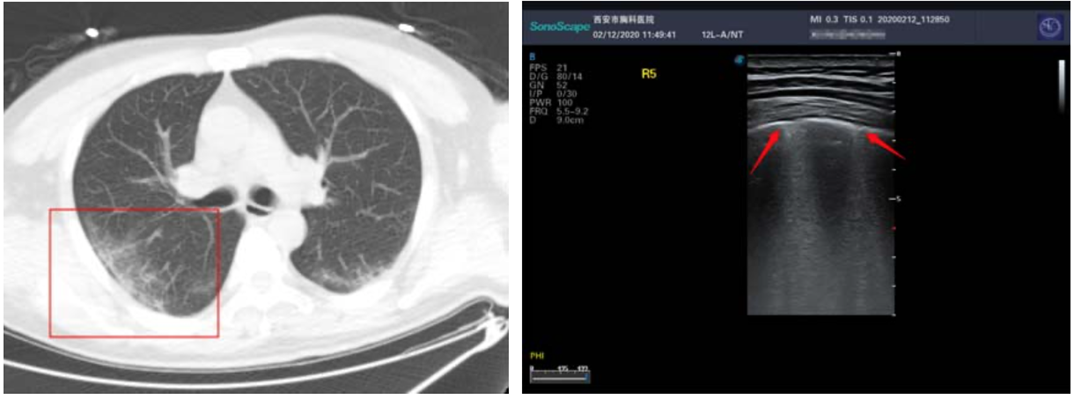
Above: A CT scan and ultrasound scan from one patient with COVID-19. Below: A CT scan and ultrasound scan from a second patient with COVID-19. All images published in SSRN and courtesy of Yi Huang and colleagues.
During the early stages of COVID-19, patients tended to exhibit focal B-line patterns, followed by alveolar interstitial syndrome as the disease progressed. In patients who were critically ill, ultrasound scans showed A-line patterns in the convalescence. For patients with pulmonary fibrosis, the scans found pleural line thickening with uneven B-line patterns.
"The findings of lung ultrasonography features of [COVID-19] are related to the stage of disease, the severity of lung injury, and comorbidities," the authors wrote. "The predominant pattern is of varying degrees of interstitial syndrome and alveolar consolidation, the degree of which is correlated with the severity of the lung injury."
The findings from Peng and colleagues mirror those of a previous study published on February 28 in SSRN. In the earlier study, lead author Yi Huang and colleagues used ultrasound scans for 20 patients with COVID-19 at the Xi'an Chest Hospital in Xi'an, China.
Huang and colleagues also used the 12-zone examination method and found similar ultrasound scan characteristics to Peng and colleagues. For instance, they found a higher proportion of B-line patterns in lesion areas, including fused B lines, as well as pleural lines that presented as discontinuous, interrupted, or unsmooth.
Better than CT?
The ultrasound scan findings from both studies lined up well with chest CT scans results. For instance, in Peng and colleague's study thickened pleura on CT scans presented as a thickened pleural line on ultrasound. Further, pulmonary infiltrating shadow on CT was linked to confluent B-line patterns on ultrasound.
Similarly, the chest CT scan of one patient in Huang and colleague's study showed ground-glass opacity and air bronchogram sign under the pleura of one lung (Figure 1). The ultrasound scan of the same patient revealed an uneven pleural line and B-line patterns (Figure 2).
While both sets of authors agreed that lung ultrasonography had several benefits over chest CT for patients with COVID-19, they also noted ultrasound shouldn't be used as the only imaging method. For instance, CT is still needed to identify patients who have pneumonia that does not extend to the pleural cavity,
- "Our study indicated that ultrasound can show typical manifestations and has advantages over CT in the clinical diagnosis and treatment of noncritical COVID-19, but it cannot replace CT," wrote Huang and colleagues. "Ultrasound can be used as a supplemental method."