June 4, 2021 -- Lung ultrasound with an abbreviated scanning protocol can efficiently diagnose pulmonary congestion caused by fluid overload in hemodialysis patients, according to research published June 3 in the American Journal of Kidney Diseases.
A team of researchers led by Dr. Nathaniel Reisinger from the University of Pennsylvania found that several abbreviated lung ultrasound protocols that focus on a limited number of lung zones (4, 6, or 8-zone) performed similarly to comprehensive 28-zone studies among patients with kidney failure on hemodialysis seeking care in an emergency department.
The researchers also did not find any differences in mortality between patients with no-to-mild and moderate-to-severe pulmonary congestion.
"Abbreviated lung ultrasound protocols take less time, are less bothersome to patients, and are nearly as accurate," Reisinger told AuntMinnie.com.
Pulmonary congestion from fluid overload is common among patients with kidney failure on hemodialysis and contributes to excess morbidity and mortality in patients. The team said that physical examination is an insensitive approach to detecting pulmonary congestion.
Lung ultrasound with a comprehensive 28-zone protocol has been shown to be sensitive for detecting pulmonary congestion, according to previous research. However, the 28-zone technique requires complete disrobing of the patient and longer scanning times for operators.
"In the constrained environment of the emergency department, this commitment is prohibitive to both patients and providers," the authors wrote.
Reisinger and his team wanted to see if abbreviated forms of lung ultrasound could produce similar results while saving time for operators and providing a more comfortable experience for patients.
The group started with research by Buessler and colleagues that studied the use of four-, six-, and eight-zone scanning for heart failure patients, as well as mapped the specific lung zones that would be most equivalent to a 28-zone study. The researchers noted that previous research has found that the regional distribution of pulmonary edema on imaging based on clinical condition has been well-demonstrated.
They then tested the protocol in 98 patients in the U.S. with kidney failure on hemodialysis participated, with a follow-up time of 30 days. Out of those, 84 were African American and 97 were non-Hispanic or Latino in ethnicity.
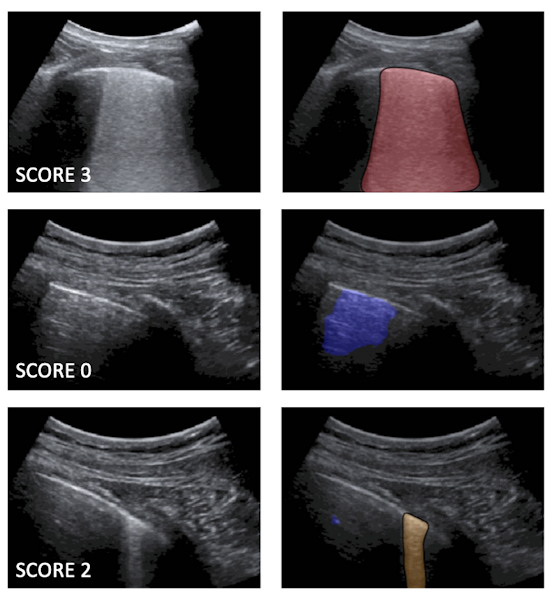
The team found high correlation and good agreement between 28-zone and abbreviated lung ultrasound studies. Each of the short-form studies was able to discriminate between no-to-mild pulmonary congestion versus moderate-to-severe pulmonary congestion when compared with the long-form 28-zone study, the authors wrote.
For short-form studies, the highest sensitivities were seen in 6C, 8C, and 8D zone ultrasound studies at 93.0%, 95.8%, and 98.6% respectively. Meanwhile, 6C and 8A studies had the highest specificities, at 96.3% and 100% respectively. Finally, 6C, 8C, and 8D studies had the highest area under the curve (AUC), at 0.95, 0.94, and 0.94 respectively.
Of the four-zone studies, lung zone 4C had the highest sensitivity at 90.1%, specificity at 92.6%, and AUC at 0.91.
"With AUC values of greater than 0.88, any of the 8-zone studies clearly seems sufficient for clinical use," the study authors wrote. "Similarly, the 4C pattern can easily be performed without removing a patient's shirt, while still achieving a point estimate of AUC greater than 0.90, demonstrating accuracy better than the current standard-of-care assessment of pulmonary congestion."
However, Reisinger said that despite the promise, abbreviated lung ultrasound protocols are "slightly less accurate" than more comprehensive tests and may miss focal pathology such as pneumonia.
He told AuntMinnie.com that the research team is looking at randomized controlled trials as the next step in investigating whether lung ultrasound-guided ultrafiltration therapy improves outcomes in patients with end-stage kidney disease chronically on hemodialysis.