Tổng số lượt xem trang
Thứ Bảy, 12 tháng 2, 2022
Thứ Năm, 3 tháng 2, 2022
POCUS can help rule out pulmonary embolism (PE) in critically ill COVID-19 patients
February 3, 2022 -- Point-of-care ultrasound (POCUS) can help rule out pulmonary embolism (PE) in critically ill COVID-19 patients when imaging multiple organs, according to Dutch research published February 2 in the Journal of Critical Care. A team led by Dr. Arthur Lieveld from Amsterdam University Medical Centers in the Netherlands wrote that POCUS could help determine which COVID-19 patients should undergo CT pulmonary angiography.
"In addition, finding right ventricular strain can make pulmonary embolism more likely in this setting, while a deep venous thrombosis would preclude the need for a CT pulmonary angiogram," Lieveld and colleagues wrote.
Critically ill COVID-19 patients have an increased risk of developing pulmonary embolism. While CT pulmonary angiography is the standard for diagnosing this, transporting patients for imaging carries health risks. CT also requires more time for decontamination and more medical personnel, which reduces time that could be dedicated toward patient care.
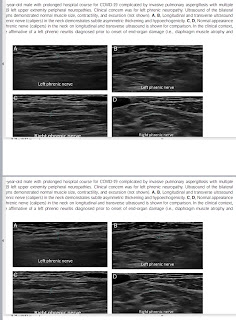
POCUS has been explored for imaging COVID-19 patients due to its portability and use for bedside imaging. While evidence is limited in detecting pulmonary embolism, some recent statements recommend using POCUS for critically ill patients.
Lieveld and colleagues wanted to find out how accurate POCUS is in diagnosing PE in these patients by looking at multiple organs together and separately. These include the lung, deep veins, and the heart.
The researchers looked at data from 70 COVID-19 patients in the intensive care unit with an average age of 67.5 years, 23 patients of whom had a pulmonary embolism. They also wrote that the median scan time with POCUS was 14 minutes.
The team found that imaging multiple organs together yielded higher accuracy than when single organs were imaged. Multiorgan POCUS had a sensitivity of 87.5% and a specificity of 25%.
POCUS' diagnostic accuracy for subpleural consolidations meanwhile was 42.9%, 75.6% for deep venous thrombosis, and 74.4% for right ventricular strain. The sensitivity and specificity for deep venous thrombosis was 24% and 88.8%, while sensitivity and specificity for right ventricular strain were 40% and 83%, respectively.
The researchers wrote that based on these results, subpleural consolidations are "hardly useful" in detecting pulmonary embolisms. However, they added that the high sensitivity displayed by multiorgan POCUS, which includes these consolidations, means this method may have a role in ruling out pulmonary embolism.
"The main driver of the good sensitivity seems to be subpleural consolidations, which ... seem to be ubiquitous in critically ill COVID-19 patients," the study authors wrote.
They also wrote that POCUS could remove some socioeconomic barriers as an affordable, easy-to-use tool for timely imaging.
"Moreover, it is easy to learn for [para]medical personnel," researchers added. "In our study, all POCUS scans were performed by intensive care unit residents. Considering that nonspecialist physicians see and treat the bulk of COVID-19 patients, this underscores the applicability of POCUS in a real-life setting."