October 19, 2022 -- Calibrated ultrasound can help with disease staging in hepatic steatosis by detecting liver fat, with results comparable to that of liver biopsy, according to Dutch research published October 18 in Radiology.
A team led by Dr. Gert Weijers from the Radbound Institute for Health Sciences said that the study results show that their calibrated ultrasound method can serve as a noninvasive alternative for liver disease screening and monitoring.
"With the growing epidemic of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis, the need has emerged for an accessible and safe diagnostic measure to screen and observe patients with steatosis," Weijers et al wrote.
Nonalcoholic fatty liver disease is a tricky challenge to pinpoint, which starts with fat accumulation in the liver. Accumulation at 5% or higher being considered steatosis. This disease can progress to nonalcoholic steatohepatitis, which includes inflammation and hepatocyte injury with or without fibrosis and eventual cirrhosis.
Liver biopsy is the standard for staging steatosis, but researchers wrote that this is invasive and can have complications. Although MRI has shown promise in noninvasive screening and monitoring, it's costly and time-consuming, according to the researchers.
The team wanted to look at the diagnostic performance of their calibrated ultrasound protocol for detecting and staging hepatic steatosis. They validated their method against liver biopsy as a reference standard.
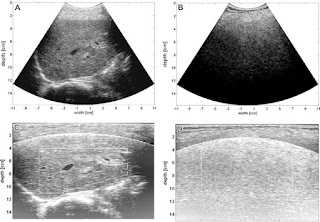
The protocol uses conventional 2D ultrasound B-mode images and semiautomatically estimates echo-level and texture parameters. The researchers noted particular interest in the residual attenuation coefficient (RAC), which is the remaining steatosis-driven attenuation gathered after beam profile correction. Data were correlated with patient characteristics, steatosis grades, and fibrosis stages.
"The method is generic, requires only a fixed imaging preset on the ultrasound system, that has been calibrated once, using a tissue-mimicking phantom," Weijers told AuntMinnie.com. "The exported 2D images obtained using this preset can be loaded and analyzed in the calibrated ultrasound software, which runs on a laptop or personal computer."
The study authors put their protocol to the test by examining images collected between 2012 and 2016 from a total of 195 patients, of which 110 were men. Out of the total, 97 patients were placed into a training set while the remaining 98 were placed in a test set. Two observers analyzed the imaging data.
The team found that the average calibrated ultrasound interobserver correlation coefficient was 0.95, and that the best correlation with steatosis was found for the RAC parameter (r = 0.78, p < 0.01). However, no correlation was found for fibrosis (r = 0.14, p = 0.054).
Additionally, steatosis detection using RAC showed an area under the receiver operating curve (AUC) of 0.97, with the same going for multivariable AUC. The researchers also noted that the predictive performance for moderate and severe hepatic steatosis using RAC was 0.93 and 0.93, respectively.
They noted a few reasons for the high performance of calibrated ultrasound in the study. For one, this method automatically assesses a large region of the ultrasound image and makes up for the normal depth-dependent behavior of the ultrasound beam and angle dependencies. As a result, it yields depth-independent analysis of quantitative ultrasound parameters.
"Further, automatic segmentation of large blood vessels and the bile duct avoids the impact of vessel wall reflections and blood signals on the calibrated ultrasound parameter," they added.
The group also highlighted that this protocol could enable clinicians to provide feedback on lifestyle changes and may be used as an outcome in clinical trials investigating new therapeutic drugs for nonalcoholic fatty liver disease.
“We also are training and testing convolutional neural networks for steatosis detection in order to enable real-time detection of steatosis on handheld ultrasound devices, to make screening- and follow-up applications accessible and affordable on a large scale,” Weijers added.
Không có nhận xét nào :
Đăng nhận xét