Tổng số lượt xem trang
Thứ Hai, 25 tháng 6, 2018
Thứ Sáu, 22 tháng 6, 2018
I B D in Children and Ultrasound
Abstract
Background
Magnetic resonance enterography (MRE) is the current gold standard for imaging in inflammatory bowel disease, but ultrasound (US) is a potential alternative.
Objective
To determine whether US is as good as MRE for the detecting inflamed bowel, using a combined consensus score as the reference standard.
Materials and methods
We conducted a retrospective cohort study in children and adolescents under 18 years with inflammatory bowel disease (IBD) at a tertiary and quaternary centre. We included children who underwent MRE and US within 4 weeks. We scored MRE using the London score and US using a score adapted from the METRIC (MR Enterography or Ultrasound in Crohn’s Disease) trial. Four gastroenterologists assessed an independent clinical consensus score. A combined consensus score using the imaging and clinical scores was agreed upon and used as the reference standard to compare MRE with US.
Results
We included 53 children. At a whole-patient level, MRE scores were 2% higher than US scores. We used Lin coefficient to assess inter-observer variability. The repeatability of MRE scores was poor (Lin 0.6). Agreement for US scoring was substantial (Lin 0.95). There was a significant positive correlation between MRE and clinical consensus scores (Spearman’s rho = 0.598, P=0.0053) and US and clinical consensus scores (Spearman’s rho = 0.657, P=0.0016).
Conclusion
US detects as much clinically significant bowel disease as MRE. It is possible that MRE overestimates the presence of disease when using a scoring system. This study demonstrates the feasibility of using a clinical consensus reference standard in paediatric IBD imaging studies.
Keywords
Adolescents Children Diagnostic accuracy Inflammatory bowel disease Magnetic resonance imaging Reproducibility UltrasoundThứ Năm, 21 tháng 6, 2018
Elastography of the GI Tract.
Odd Helge Gilja, Prof., MD, PhD National Centre for Ultrasound in Gastroenterology Haukeland University Hospital, Bergen, and Department of Clinical Medicine, University of Bergen, Norway.
Elastography is a relative new technique that depicts the stiffness of tissue and is already used in clinical practice for several indications.
Guidelines and recommendations of the different techniques and clinical applications was published by EFSUMB. Elastography and strain imaging has also been suggested as a tool for assessing diseases of the gastrointestinal tract.
The bowel wall is a thin structure, which does not make it the ideal organ to be studied with elastography. However, pathology of the GI tract such as inflammation or tumour causes bowel wall thickening and often reduces motility and luminal contents in the affected area which may facilitate strain imaging. There is evidence for the use of elastography in endorectal ultrasonography, but the evidence for transabdominal elastography of the bowel is sparse. However, some recent studies suggest that it can be used to differentiate between fibrotic and inflammatory stenosis in Crohn’s disease. In patients with a stricture of the bowel and resultant bowel obstruction, it is important to determine if there is active inflammation at the site of stricture or if the obstructed segment is fibrotic. Using elastography, the active inflammatory components will be softer whereas the fibrotic stricture will appear stiffer. Accordingly, one may apply elastography to evaluate stiffness of the stenotic area, thus providing more clues to the fibrous content of the stricture. In conclusion, elastography may become a relevant clinical tool, but we need more studies to determine its usefulness in the management of patients with GI diseases.
References: 1. Bamber J, Cosgrove D, Dietrich CF, Fromageau J, Bojunga J, Calliada F, Cantisani V, Correas JM, D’Onofrio M, Drakonaki EE, Fink M, Friedrich-Rust M, Gilja OH,Havre RF,JenssenC,KlauserAS,Ohlinger R, Saftoiu A,SchaeferF, SporeaI,PiscagliaF. EFSUMBGuidelinesand Recommendations on the Clinical Use of Ultrasound Elastography. Part 1: Basic Principles and Technology. Ultraschall Med. 2013 Apr;34(2):169-84. http://dx.doi.org/10.1055/s-00331335205. Epub 2013 Apr 4. 2. Cosgrove D, Piscaglia F, Bamber J, Bojunga J, Correas JM, Gilja OH, Klauser AS, Sporea I, Calliada F, Cantisani V, D’Onofrio M, Drakonaki EE, Fink M, Friedrich-Rust M, Fromageau J, Havre RF, Jenssen C, Ohlinger R, Saftoiu A, Schaefer F, Dietrich CF. EFSUMBGuidelines and Recommendations on the Clinical Use of Ultrasound Elastography.
Elastography is a relative new technique that depicts the stiffness of tissue and is already used in clinical practice for several indications.
Guidelines and recommendations of the different techniques and clinical applications was published by EFSUMB. Elastography and strain imaging has also been suggested as a tool for assessing diseases of the gastrointestinal tract.
The bowel wall is a thin structure, which does not make it the ideal organ to be studied with elastography. However, pathology of the GI tract such as inflammation or tumour causes bowel wall thickening and often reduces motility and luminal contents in the affected area which may facilitate strain imaging. There is evidence for the use of elastography in endorectal ultrasonography, but the evidence for transabdominal elastography of the bowel is sparse. However, some recent studies suggest that it can be used to differentiate between fibrotic and inflammatory stenosis in Crohn’s disease. In patients with a stricture of the bowel and resultant bowel obstruction, it is important to determine if there is active inflammation at the site of stricture or if the obstructed segment is fibrotic. Using elastography, the active inflammatory components will be softer whereas the fibrotic stricture will appear stiffer. Accordingly, one may apply elastography to evaluate stiffness of the stenotic area, thus providing more clues to the fibrous content of the stricture. In conclusion, elastography may become a relevant clinical tool, but we need more studies to determine its usefulness in the management of patients with GI diseases.
References: 1. Bamber J, Cosgrove D, Dietrich CF, Fromageau J, Bojunga J, Calliada F, Cantisani V, Correas JM, D’Onofrio M, Drakonaki EE, Fink M, Friedrich-Rust M, Gilja OH,Havre RF,JenssenC,KlauserAS,Ohlinger R, Saftoiu A,SchaeferF, SporeaI,PiscagliaF. EFSUMBGuidelinesand Recommendations on the Clinical Use of Ultrasound Elastography. Part 1: Basic Principles and Technology. Ultraschall Med. 2013 Apr;34(2):169-84. http://dx.doi.org/10.1055/s-00331335205. Epub 2013 Apr 4. 2. Cosgrove D, Piscaglia F, Bamber J, Bojunga J, Correas JM, Gilja OH, Klauser AS, Sporea I, Calliada F, Cantisani V, D’Onofrio M, Drakonaki EE, Fink M, Friedrich-Rust M, Fromageau J, Havre RF, Jenssen C, Ohlinger R, Saftoiu A, Schaefer F, Dietrich CF. EFSUMBGuidelines and Recommendations on the Clinical Use of Ultrasound Elastography.
Thứ Tư, 20 tháng 6, 2018
Ultrasound links meat allergen to heart disease
By Kate Madden Yee, AuntMinnie.com staff writer
June 15, 2018 -- Using intravascular ultrasound (IVUS), researchers from the U.S. National Institutes of Health (NIH) have found a link between sensitivity to an allergen in red meat and plaque buildup in the heart's arteries, according to a study published online June 14 in Arteriosclerosis, Thrombosis, and Vascular Biology.
Only recently have scientists identified the main allergen in red meat, called galactose-alpha-1,3-galactose, or alpha-Gal, wrote a team led by Dr. Coleen McNamara from the University of Virginia Health System. It's also been discovered that the lone star tick, found predominately in the southeastern U.S., sensitizes people to this allergen when it bites them, boosting the incidence of meat allergies in this area.
Researchers have suspected for some time that allergens can trigger immunological changes that may be associated with plaque buildup and artery blockages. In their study, McNamara and colleagues showed that a type of antibody (immunoglobulin) specific to the alpha-Gal allergen was associated with higher levels of arterial plaque.
The investigators analyzed blood samples from 118 adults and found antibodies to alpha-Gal in 26%. Next, they used intravascular ultrasound (IVUS) to analyze the quantity of plaque in the blood samples. The amount was 30% higher in the alpha-Gal-sensitized patients than in the nonsensitized patients.
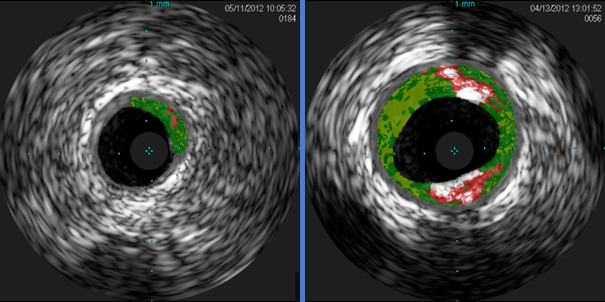
Cross-sectional IVUS images of coronary arteries. Plaque buildup (colored areas) in an artery from a patient who lacks sensitivity to the red meat allergen (left) is much lower than plaque levels in an artery from a patient with sensitivity to the allergen (right). Images courtesy of Dr. Angela Taylor of the University of Virginia Health System.
"This novel finding from a small group of subjects from Virginia raises the intriguing possibility that allergy to red meat may be an underrecognized factor in heart disease," McNamara said in a statement released by the NIH. "These preliminary findings underscore the need for further clinical studies in larger populations from diverse geographic regions and additional laboratory work."
Thứ Sáu, 15 tháng 6, 2018
Stress echo beats CCTA for evaluating chest pain
June 13, 2018 -- Stress echocardiography is a safe method of evaluating chest pain in patients who present to the emergency department, resulting in lower rates of hospitalization and shorter hospital stays when compared with coronary CT angiography (CCTA), according to a study published online June 13 in JACC: Cardiovascular Imaging.
The findings suggest that stress echo could be an effective alternative to CCTA for emergency department (ED) chest pain triage, reducing patients' radiation exposure and healthcare costs. But the modality is often disregarded as an option, wrote a team led by Dr. Jeffrey Levsky, PhD, from Albert Einstein College of Medicine in New York City.
"[Concerns] regarding CCTA use include radiation exposure, increased subsequent noninvasive testing ... increased catheterization and coronary revascularization of uncertain benefit, increased downstream clinical resource utilization, and the burden inherent to incidental findings," the group wrote. "Each of these concerns is addressed by the alternative use of stress echocardiography, a modality that has been assessed in early emergency department triage but is often overlooked."
Better assessment?
Cardiovascular disease causes one of three deaths worldwide, Levsky and colleagues wrote. Chest pain is a common reason patients present in the emergency department due to concerns that the pain signifies a heart attack. There are a number of ways to assess chest pain, but CCTA is quick and has been shown to reduce a patient's stay in the hospital compared to other modalities such as nuclear myocardial perfusion imaging (MPI)

Dr. Jeffrey Levsky, PhD, from Albert Einstein College of Medicine.
"We conducted this study because there are very few published trials that rigorously compare different ways to work up emergency department chest pain patients," Levsky told AuntMinnie.com. "Chest pain is such an important emergency presentation -- involving literally millions of Americans yearly -- but assessing it can take a lot of time and expense."
CCTA exposes patients to radiation, however, and it can prompt further procedures that may or may not be of benefit, the group noted. That's why stress echocardiography shows promise for evaluating chest pain in the emergency department, although it does have its challenges.
"Stress echo requires close coordination of the exercise and imaging parts and a good deal of patient cooperation," he said. "Critics of the technique feel it is too low in sensitivity. But on the other hand, it does not require radiation, and long-term outcomes are good when the test is negative."
Levsky and colleagues started with 400 low- to intermediate-risk acute chest pain patients who presented to the emergency department between August 2011 and January 2016 and randomized them to CCTA (201 patients) or stress echocardiography (199 patients). The patients had no known coronary artery disease and had negative initial serum troponin levels. The study's primary outcome measure was the hospitalization rate, while its secondary end point was the length of stay in the emergency department and/or the hospital. Of the subjects, 42.5% were women and 87.3% were ethnic minorities, the group wrote.
The researchers found that patients who underwent stress echocardiography had lower rates of hospitalization, shorter emergency department and hospital stays, and fewer adverse events on follow-up (although this last metric was not statistically significant).
| Comparison of CCTA vs. stress echo for chest pain | ||||
| Measure | CCTA | Stress echocardiography | Change | p-value |
| Hospitalized on arrival at ED | 19% | 11% | -8 percentage point change | 0.026 |
| Median ED stay | 5.4 hours | 4.7 hours | -13% | < 0.001 |
| Median hospital stay | 58 hours | 34 hours | -41% | 0.002 |
| Adverse events over a median 24 months of follow-up | 11 | 7 | -36% | 0.47 |
| Median initial workup radiation exposure | 6.5 mSv | None | -100% | N/A |
"[Our study] provides the first comparison of CCTA and stress echocardiography in emergency department chest pain patients and shows a statistically significant 8% reduction of hospitalization in patients triaged with stress echocardiography compared to CCTA," the group wrote.
The researchers also found an overall trend toward less resource utilization over a 24-month follow-up period among patients who underwent stress echocardiography, although most measures did not reach statistical significance. There was no statistically significant difference between CCTA and stress echocardiography regarding subsequent catheterization and revascularization, and patients rated their experience with stress echocardiography more favorably than with CCTA.
An effective tool
Stress echocardiography appears to be a safe and effective tool for evaluating chest pain in the emergency department compared with CCTA, Levsky and colleagues wrote.
"Stress echocardiography resulted in the discharge of a significantly higher number of patients with significantly shorter lengths of stay, was safe at intermediate-term follow-up, and provided a better patient experience," they concluded.
Letters blast study linking ultrasound and autism
June 11, 2018 -- A study published in February in JAMA Pediatrics that suggested a link between the incidence of autism spectrum disorder (ASD) and prenatal ultrasound is coming under fire by critics who are calling out the study's conclusion as oversimplified at best and inaccurate at worst
The original research, conducted by a team led by Dr. N. Paul Rosman of Boston Medical Center, claimed to find a statistically significant association between the development of ASD and one technical sonography parameter: the depth of ultrasound penetration for scans performed at certain points during pregnancy.
But this measure isn't valid, wrote Dr. Christoph Lees from the Imperial College Healthcare NHS Trust in London in a letter published online June 11, also in JAMA Pediatrics.
"The authors introduce a hitherto unheard-of index: the depth of ultrasonographic penetration," he wrote. "This has no clear biological or scientific justification. Nevertheless, they report that the mean depth of penetration of the ultrasound beam is greater in those who developed ASD than in healthy children. But depth of penetration of ultrasound is not a measure of ultrasonography exposure; it simply tells us how far the ultrasound beam reaches."
The study authors' conclusion that "further research is needed to determine whether other variables of ultrasound exposure also have adverse effects on the developing fetus" doesn't accurately reflect the data, he wrote.
"In apparent contravention of JAMA Pediatrics' guidance for reporting clinical studies of this nature, no recruitment flowchart with participant exclusion/inclusion criteria is shown, and neither a priori hypothesis, predefined primary outcome, nor sample size calculation are included," Lees wrote.
The study also drew criticism in a letter from Drs. David Somerset and Robert Wilson of the University of Calgary, who believe the study's conclusion that "greater ultrasonographic depth" negatively affects the fetus has not been proved and is a "gross oversimplification."
"The authors present no evidence that a mean difference of 4 mm in depth is associated with higher energy delivery to the fetus," they wrote. "Furthermore, clinical variables, such as maternal obesity and age and paternal age, are independently associated with ASD ... and these variables have not been accounted for. It is a shame that ... [the] study has such an alarmist conclusion in the abstract that is not supported by the study findings."
Because possible links between ultrasound and autism cause such anxiety among parents and pregnant women, it's crucial that studies are reported accurately, Lees concluded.
"In fact, this study shows that children with ASD were exposed to a shorter duration of prenatal ultrasonography and lower-energy scans than healthy children," he wrote. "These findings are reassuring. We respectfully suggest that a more accurate form of words would have reflected the study's finding than is found in the conclusion of the abstract.
Thứ Năm, 7 tháng 6, 2018
Thứ Tư, 6 tháng 6, 2018
POCUS helps medical students find more AAAs than surgeons
June 1, 2018 -- With a bit of training, medical students using point-of-care ultrasound (POCUS) can identify more abdominal aortic aneurysms (AAAs) than vascular surgeons can by screening for the condition via physical exam, according to a study published online May 17 in the Annals of Vascular Surgery.
The findings not only confirm ultrasound's efficacy for this application but also suggest a new resource for AAA screening in an era when medical staff can be stretched thin, wrote the team led by Trinh Mai from the University of Ottawa.
"Screening for AAA has been found to be largely underutilized in the U.S., with only 15% of eligible and at-risk individuals receiving screening examinations," the researchers wrote. "To mitigate obstacles associated with access to screening [such as staff and device availability] ... the introduction of point-of-care ultrasound training at the medical student level, and its wide-scale implementation as an extension to physical examination, may lead to improved detection of AAA."
Ultrasound training
When untreated, abdominal aortic aneurysms have a mortality rate as high as 85% to 90%, Mai and colleagues wrote. Physical examination has low sensitivity and specificity, even when experienced physicians perform it.
Ultrasound is much more effective and is currently the primary imaging tool used to screen for the condition, but its widespread use for this application has been hindered by cost and the availability of appropriately trained technicians.
However, there's mounting evidence that medical personnel with no previous training can effectively use ultrasound to screen for AAA, especially with point-of-care ultrasound.
"The objective of our study was to determine whether a medical student, after a short training period, could reliably screen for abdominal aortic aneurysms," the group wrote. "We compared the test characteristics of point-of-care ultrasound performed by a medical student versus physical examination by vascular surgeons and a gold standard reference scan."
For the study, the researchers included data from 57 patients who presented to an outpatient vascular surgery clinic between October 2015 and March 2016 to be screened for abdominal aortic aneurysm. A vascular surgeon evaluated each patient via physical exam, followed by a second-year medical student using POCUS; patients then underwent a reference CT or vascular sonographer-performed ultrasound exam within three months of this initial screening visit.
The student had three hours of training with POCUS for detecting and measuring AAA. The training included a theoretical component led by a vascular sonographer and a practical component taught by an emergency physician, during which the student practiced ultrasound scanning under direct guidance.
After this initial training, the student practiced using ultrasound on the abdominal aortas of 60 patients with and without the condition. The student then completed a competency assessment before beginning to scan study participants, Mai and colleagues wrote.
Most of the patients (61%) were men, and the median patient age was 71. Reference exams identified 16 abdominal aortic aneurysms with a mean maximum aortic diameter of 29.5 mm. Of these, the vascular surgeon identified 11, with two false positives, for a sensitivity rate of 66.7% and a specificity rate of 94.4%. The average time to conduct the physical exam was 35 seconds.
Medical students using point-of-care ultrasound found 15 of the 16 abdominal aortic aneurysms with a mean maximum aortic diameter of 28 mm, for a sensitivity rate of 93.3% and a specificity rate of 100%. The average time to conduct the ultrasound exam was four minutes, the group wrote.
| Physical exam vs. POCUS for AAA screening | ||
| Measure | Physical exam | Point-of-care ultrasound |
| Sensitivity | 68.8% | 93.8% |
| Specificity | 93.9% | 100% |
| Positive predictive value | 81.8% | 100% |
"The results of our study, as well as several others, have proven that physical examination is relatively unreliable for the detection of abdominal aortic aneurysms," the researchers noted. "Screening for abdominal aortic aneurysms may be accurately and efficiently performed by a novice operator using point-of-care ultrasound with relatively limited training and experience."
Core curriculum?
Because point-of-care ultrasound appears to be an effective tool for identifying AAA, perhaps its use should be more formally incorporated into the medical school curriculum, Mai's team suggested.
"This study raises the question of whether we should be changing the way we are teaching medical students," the group wrote. "With the increased prevalence and use of ultrasound in medical practice, perhaps we should consider teaching focused ultrasound for abdominal aortic aneurysm detection as a standard in the medical school curriculum."
Thứ Bảy, 2 tháng 6, 2018
Thứ Năm, 31 tháng 5, 2018
Cesarean delivery changes the uterine angle
May 30, 2018 -- Cesarean delivery can change the angle of a woman's uterus from an anteflexed one, in which the fundus faces the abdominal wall, to a retroflexed one, in which it faces the sacrum, according to a study in the May issue of the Journal of Ultrasound in Medicine
Because a retroflexed uterus can increase a woman's risk of uterine perforation during gynecologic surgery or the placement of an intrauterine device (IUD), the angle of her uterus after cesarean must be determined via ultrasound, wrote a team led by Dr. Andrea Agten of St. George's University Hospitals in London.
"Over the years, reports have associated a retroflexed uterine position with an increased surgical complication rate (e.g., uterine perforation) ... [and] although in many cases perforations are innocuous, some lead to infections, hemorrhage, and trauma to other abdominal organs," Agten and colleagues noted. "Therefore, all women with a history of cesarean delivery should undergo a transvaginal ultrasound examination before any gynecologic surgery or IUD placement" (J Ultrasound Med, May 2018, Vol. 37:5, pp. 1179-1183)
Which angle?
One of the ways the position of the uterus is assessed is by its flexion angle, which is the measure between the uterus and the cervix. Gauging uterine position is crucial for successful gynecologic procedures such as dilation and curettage, endometrial biopsy, and IUD insertion, the team wrote.
The researchers conducted the study because they had observed an increase in retroflexed uteri in their practice. And because the number of cesarean deliveries has also increased, they sought to investigate whether this higher incidence of retroflexed uterus could be caused by cesarean delivery.
The study included data from 173 patients who had undergone transvaginal ultrasound before and after either vaginal or cesarean delivery between 2012 and 2015, excluding women who had undergone a previous cesarean delivery. Two radiologist readers measured flexion angles from these exams before and after the women gave birth, and they compared them between women with vaginal and cesarean deliveries.
Of the 173 women, 107 had vaginal deliveries (62%) and 66 had cesareans (38%). The mean interval between scans was 18 months; interreader agreement for flexion angles was almost perfect, the researchers found (0.939 before delivery and 0.969 after, p < 0.001).
There was no significant difference in mean flexion angles between the uterus and the cervix for either type of delivery on antepartum ultrasound (145.8° for vaginal delivery and 154.8° for cesarean). But mean postpartum flexion angles increased significantly after cesarean, at 152.8° for women who had a vaginal delivery compared with 180.4° for those who underwent a cesarean (p < 0.001).
The change in flexion angle translated into a shift from anteflexed to retroflexed in more of the women who underwent cesarean delivery than those who had a vaginal delivery (29% versus 13%, p = 0.003).
"Our study showed that cesarean delivery can change the natural position of the uterus ... [and that it was] associated with the new development of a retroflexed uterus in one-third of our patients," Agten's group wrote.
Avoiding complications
Because a retroflexed uterine position has been associated with surgical complications, it's important for a woman's health going forward to assess the position of her uterus after she has had a cesarean, Agten and colleagues wrote.
"Cesarean delivery can change the uterine flexion angle to a more retroflexed position," the researchers concluded. "Therefore, all women with a history of cesarean delivery should undergo a transvaginal sonography examination before any gynecologic surgery or IUD placement to reduce the possibility of surgical complications.
Thứ Tư, 30 tháng 5, 2018
Can AI reliably measure carotid intima-media thickness?
By Erik L. Ridley, AuntMinnie staff writer
May 25, 2018 -- Artificial intelligence (AI) software that combines deep-learning and machine-learning techniques can measure carotid intima-media thickness (CIMT) more accurately than sonographers can, according to research in the July 1 issue of Computers in Biology and Medicine.
In testing, a multi-institutional and multinational team led by Mainak Biswas of the National Institute of Technology Goa in India found that its deep learning-based model outperformed previous automated methods. The model was also up to 20% more accurate than sonographers in measuring CIMT, an important biomarker for cardiovascular disease and stroke monitoring.
"The results showed that the performance of the [deep learning]-based approach was superior to the nonintelligence-based conventional methods that use spatial intensities alone," the authors wrote. "The [deep-learning] system can be used for stroke risk assessment during routine or clinical trial modes."
An important biomarker
An increase in CIMT -- the mean perpendicular distance between the lumen-intima (LI) and the media-adventitia (MA) interfaces -- has been associated with an increased risk of cardiovascular events and stroke. However, the current process of measuring CIMT suffers from accuracy and reproducibility issues due to factors such as variability in patient nationality, ethnicity, disease, and age group. Technical challenges also play a role; traditional manual segmentation of these regions is slow, error-prone, and subject to intraobserver and interobserver variability, according to the researchers (Comput Biol Med, July 1, 2018, Vol. 98, pp. 100-117).
As a result, a number of automated techniques have been developed for predicting CIMT, using various spatial features such as grayscale median, pixel classification, gradient edges, space-scale, or a combination of these features, the researchers explained.
"Despite their strong contributions, these external factors make the spatial-based methods prone to variability and a lack of robustness when it comes to completely automated designs," they wrote.
Biswas and colleagues hypothesized that a deep-learning system would be more reliable and accurate than previous methods, thanks to its inherent ability to provide better regional segmentation output. To train and test a deep-learning model, the researchers used 396 high-resolution B-mode ultrasound images of the right and left common carotid artery from 203 patients at Toho University in Japan. The ultrasound scans were obtained on one of three ultrasound systems (Aplio XV, Aplio XG, and Xario) from Canon Medical Systems. Of the 396 images, 90% were used for training the deep-learning model and 10% were set aside for testing.
Manual tracing of the lumen and adventitia borders was performed using ImgTracer software (AtheroPoint). Dr. Jasjit Suri, PhD, from AtheroPoint served as senior author on the study.
A 2-stage system
The researchers developed a two-stage system that made use of both deep and machine learning. In the first stage, a convolution layer-based encoder was used to extract image features, while a decoder based on a fully convolutional neural network (CNN) performed image segmentation. The raw inner lumen borders and raw outer interadventitial borders generated during this process were then smoothed with a machine learning-based method. The model utilized these final borders to calculate CIMT values from the LI and MA far walls using the standardized polyline distance metric method.
As two different sets of gold standards -- lumen regional information and interadventitial regional information -- were used during the design of the deep-learning model, the researchers trained and evaluated two different algorithms. Compared with the gold standard, the two deep-learning algorithms yielded CIMT error rates of 0.126 ± 0.134 mm and 0.124 ± 1.0 mm. They also significantly outperformed previously developed systems for measuring CIMT, according to the researchers.
Biswas and colleagues also compared the performance of the deep-learning algorithms with mean far-wall CIMT measurements calculated by sonographers in 346 images. Both models correlated better with the ground truth than the sonographer measurements, which had been performed in real-time in the institution's vascular ultrasound laboratory.
| Coefficient of correlation with ground truth | |||
| Manual sonographer measurement of CIMT | Deep-learning method | Improvement of deep-learning method over sonographer measurement | |
| Ground truth 1 | 0.80 | Model 1: 0.96 | 20% |
| Ground truth 2 | 0.83 | Model 2: 0.95 | 14.5% |
The deep-learning method takes only a few milliseconds to perform, according to the researchers. They acknowledged, though, that the system relied on a dataset limited to a Japanese diabetic cohort, and it has not been tested on a wide variety of datasets.
As a result, it needs to be evaluated further in a multiethnic patient population with subclinical atherosclerosis and low-, moderate-, and high-risk scenarios, they wrote. The approach must also be evaluated on ultrasound images from different equipment vendors, and it should also be extended from a desktop PC-based application to a web-based version, according to the group.
Đăng ký:
Bài đăng
(
Atom
)

















