| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Tổng số lượt xem trang
Thứ Hai, 25 tháng 6, 2018
Thứ Sáu, 22 tháng 6, 2018
I B D in Children and Ultrasound
Abstract
Background
Magnetic resonance enterography (MRE) is the current gold standard for imaging in inflammatory bowel disease, but ultrasound (US) is a potential alternative.
Objective
To determine whether US is as good as MRE for the detecting inflamed bowel, using a combined consensus score as the reference standard.
Materials and methods
We conducted a retrospective cohort study in children and adolescents under 18 years with inflammatory bowel disease (IBD) at a tertiary and quaternary centre. We included children who underwent MRE and US within 4 weeks. We scored MRE using the London score and US using a score adapted from the METRIC (MR Enterography or Ultrasound in Crohn’s Disease) trial. Four gastroenterologists assessed an independent clinical consensus score. A combined consensus score using the imaging and clinical scores was agreed upon and used as the reference standard to compare MRE with US.
Results
We included 53 children. At a whole-patient level, MRE scores were 2% higher than US scores. We used Lin coefficient to assess inter-observer variability. The repeatability of MRE scores was poor (Lin 0.6). Agreement for US scoring was substantial (Lin 0.95). There was a significant positive correlation between MRE and clinical consensus scores (Spearman’s rho = 0.598, P=0.0053) and US and clinical consensus scores (Spearman’s rho = 0.657, P=0.0016).
Conclusion
US detects as much clinically significant bowel disease as MRE. It is possible that MRE overestimates the presence of disease when using a scoring system. This study demonstrates the feasibility of using a clinical consensus reference standard in paediatric IBD imaging studies.
Keywords
Adolescents Children Diagnostic accuracy Inflammatory bowel disease Magnetic resonance imaging Reproducibility UltrasoundThứ Năm, 21 tháng 6, 2018
Elastography of the GI Tract.
Odd Helge Gilja, Prof., MD, PhD National Centre for Ultrasound in Gastroenterology Haukeland University Hospital, Bergen, and Department of Clinical Medicine, University of Bergen, Norway.
Elastography is a relative new technique that depicts the stiffness of tissue and is already used in clinical practice for several indications.
Guidelines and recommendations of the different techniques and clinical applications was published by EFSUMB. Elastography and strain imaging has also been suggested as a tool for assessing diseases of the gastrointestinal tract.
The bowel wall is a thin structure, which does not make it the ideal organ to be studied with elastography. However, pathology of the GI tract such as inflammation or tumour causes bowel wall thickening and often reduces motility and luminal contents in the affected area which may facilitate strain imaging. There is evidence for the use of elastography in endorectal ultrasonography, but the evidence for transabdominal elastography of the bowel is sparse. However, some recent studies suggest that it can be used to differentiate between fibrotic and inflammatory stenosis in Crohn’s disease. In patients with a stricture of the bowel and resultant bowel obstruction, it is important to determine if there is active inflammation at the site of stricture or if the obstructed segment is fibrotic. Using elastography, the active inflammatory components will be softer whereas the fibrotic stricture will appear stiffer. Accordingly, one may apply elastography to evaluate stiffness of the stenotic area, thus providing more clues to the fibrous content of the stricture. In conclusion, elastography may become a relevant clinical tool, but we need more studies to determine its usefulness in the management of patients with GI diseases.
References: 1. Bamber J, Cosgrove D, Dietrich CF, Fromageau J, Bojunga J, Calliada F, Cantisani V, Correas JM, D’Onofrio M, Drakonaki EE, Fink M, Friedrich-Rust M, Gilja OH,Havre RF,JenssenC,KlauserAS,Ohlinger R, Saftoiu A,SchaeferF, SporeaI,PiscagliaF. EFSUMBGuidelinesand Recommendations on the Clinical Use of Ultrasound Elastography. Part 1: Basic Principles and Technology. Ultraschall Med. 2013 Apr;34(2):169-84. http://dx.doi.org/10.1055/s-00331335205. Epub 2013 Apr 4. 2. Cosgrove D, Piscaglia F, Bamber J, Bojunga J, Correas JM, Gilja OH, Klauser AS, Sporea I, Calliada F, Cantisani V, D’Onofrio M, Drakonaki EE, Fink M, Friedrich-Rust M, Fromageau J, Havre RF, Jenssen C, Ohlinger R, Saftoiu A, Schaefer F, Dietrich CF. EFSUMBGuidelines and Recommendations on the Clinical Use of Ultrasound Elastography.
Elastography is a relative new technique that depicts the stiffness of tissue and is already used in clinical practice for several indications.
Guidelines and recommendations of the different techniques and clinical applications was published by EFSUMB. Elastography and strain imaging has also been suggested as a tool for assessing diseases of the gastrointestinal tract.
The bowel wall is a thin structure, which does not make it the ideal organ to be studied with elastography. However, pathology of the GI tract such as inflammation or tumour causes bowel wall thickening and often reduces motility and luminal contents in the affected area which may facilitate strain imaging. There is evidence for the use of elastography in endorectal ultrasonography, but the evidence for transabdominal elastography of the bowel is sparse. However, some recent studies suggest that it can be used to differentiate between fibrotic and inflammatory stenosis in Crohn’s disease. In patients with a stricture of the bowel and resultant bowel obstruction, it is important to determine if there is active inflammation at the site of stricture or if the obstructed segment is fibrotic. Using elastography, the active inflammatory components will be softer whereas the fibrotic stricture will appear stiffer. Accordingly, one may apply elastography to evaluate stiffness of the stenotic area, thus providing more clues to the fibrous content of the stricture. In conclusion, elastography may become a relevant clinical tool, but we need more studies to determine its usefulness in the management of patients with GI diseases.
References: 1. Bamber J, Cosgrove D, Dietrich CF, Fromageau J, Bojunga J, Calliada F, Cantisani V, Correas JM, D’Onofrio M, Drakonaki EE, Fink M, Friedrich-Rust M, Gilja OH,Havre RF,JenssenC,KlauserAS,Ohlinger R, Saftoiu A,SchaeferF, SporeaI,PiscagliaF. EFSUMBGuidelinesand Recommendations on the Clinical Use of Ultrasound Elastography. Part 1: Basic Principles and Technology. Ultraschall Med. 2013 Apr;34(2):169-84. http://dx.doi.org/10.1055/s-00331335205. Epub 2013 Apr 4. 2. Cosgrove D, Piscaglia F, Bamber J, Bojunga J, Correas JM, Gilja OH, Klauser AS, Sporea I, Calliada F, Cantisani V, D’Onofrio M, Drakonaki EE, Fink M, Friedrich-Rust M, Fromageau J, Havre RF, Jenssen C, Ohlinger R, Saftoiu A, Schaefer F, Dietrich CF. EFSUMBGuidelines and Recommendations on the Clinical Use of Ultrasound Elastography.
Thứ Tư, 20 tháng 6, 2018
Ultrasound links meat allergen to heart disease
By Kate Madden Yee, AuntMinnie.com staff writer
June 15, 2018 -- Using intravascular ultrasound (IVUS), researchers from the U.S. National Institutes of Health (NIH) have found a link between sensitivity to an allergen in red meat and plaque buildup in the heart's arteries, according to a study published online June 14 in Arteriosclerosis, Thrombosis, and Vascular Biology.
Only recently have scientists identified the main allergen in red meat, called galactose-alpha-1,3-galactose, or alpha-Gal, wrote a team led by Dr. Coleen McNamara from the University of Virginia Health System. It's also been discovered that the lone star tick, found predominately in the southeastern U.S., sensitizes people to this allergen when it bites them, boosting the incidence of meat allergies in this area.
Researchers have suspected for some time that allergens can trigger immunological changes that may be associated with plaque buildup and artery blockages. In their study, McNamara and colleagues showed that a type of antibody (immunoglobulin) specific to the alpha-Gal allergen was associated with higher levels of arterial plaque.
The investigators analyzed blood samples from 118 adults and found antibodies to alpha-Gal in 26%. Next, they used intravascular ultrasound (IVUS) to analyze the quantity of plaque in the blood samples. The amount was 30% higher in the alpha-Gal-sensitized patients than in the nonsensitized patients.
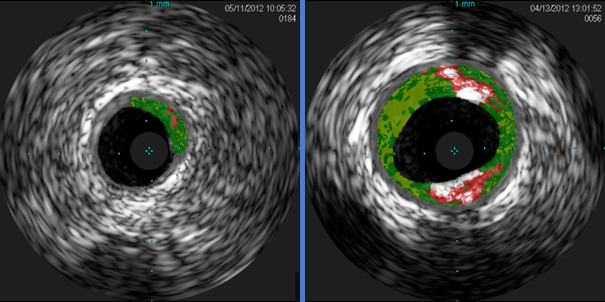
Cross-sectional IVUS images of coronary arteries. Plaque buildup (colored areas) in an artery from a patient who lacks sensitivity to the red meat allergen (left) is much lower than plaque levels in an artery from a patient with sensitivity to the allergen (right). Images courtesy of Dr. Angela Taylor of the University of Virginia Health System.
"This novel finding from a small group of subjects from Virginia raises the intriguing possibility that allergy to red meat may be an underrecognized factor in heart disease," McNamara said in a statement released by the NIH. "These preliminary findings underscore the need for further clinical studies in larger populations from diverse geographic regions and additional laboratory work."
Đăng ký:
Nhận xét
(
Atom
)