By Theresa Pablos, AuntMinnie staff writer
February 28, 2020 -- Older endurance athletes may be prone to heart conditions with a relatively high risk of death. Echocardiographic imaging helped identify an enlarged aorta in 25% of older athletes in a new study, published on February 26 in
JAMA Cardiology.
Dilation of the aorta is a risk factor for a group of related conditions tied to an in-hospital mortality rate of more than 25%, with age, male sex, and hypertension established as some risk factors for aortic dilation.
The new research suggests long-term endurance exercise may be a risk factor, too.
"Findings from this study fill an important gap in our understanding of how long-term participation in endurance sport affects the cardiovascular system," wrote the authors, led by Dr. Timothy Churchill from the cardiovascular performance program at Massachusetts General Hospital in Boston.
Previous research has found that intense exercise can contribute to aortic dilation, but no studies had looked at the impact of this phenomenon on older endurance athletes. For their study, the authors recruited 442 male and female runners and rowers who participated in competitive athletic activities, including the Boston Marathon and U.S. national-level rowing competitions.
All athletes were between the ages of 50 and 75 and had at least 10 years of endurance training after the age of 40. The authors screened out participants with a personal or family history of relevant heart conditions, including aortopathy and connective tissue disorders.
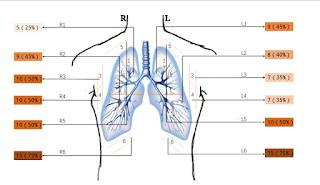
Transthoracic echocardiographic imaging was performed on the athletes to measure their myocardial structure and function. The authors took aortic measurements in triplicate over three cardiac cycles.
Out of the male athletes, almost one-third had at least one aortic dimension of 40 mm or larger; however, the findings varied by sport. Male rowers accounted for 61% of athletes with an enlarged aorta. The rowers also had a significantly larger raw aortic size and ascending aorta than male runners.
The difference in aortic dilation between male rowers and runners could be explained by the cardiovascular activity requirements of each sport, the authors noted. For instance, running requires sustained, even cardiovascular activity, whereas rowing requires different levels of strain during the stroke motion.
"While speculative, these findings suggest that the pressure stress uniquely present in rowing may represent an important hemodynamic driver of aortic dilation, particularly at the level of the aortic sinuses," the authors wrote.
For female athletes, the findings were much less pronounced. Only 6% of women had aorta measurements of 40 mm or larger, and there was no significant difference between runners and rowers. However, 38% of female athletes would meet the criteria for enlarged aorta if the threshold was lowered to 34 mm, another standard measurement.
Finally, aortic dilation was also linked to elite athlete status, defined as rowers who participated in the Olympics or world championships and marathon runners who completed races in under two hours and 45 minutes. Elite competitors and those with more cumulative years of athletic training had significantly larger aortic dimensions, the authors found.
"To our knowledge, this study presents the first detailed characterization of the prevalence of clinically relevant ascending aortic dilation among aging competitive athletes," the authors wrote.
What these findings mean for clinical outcomes has yet to be ascertained, the authors noted. They theorized the changes in aorta size could be a previously unrecognized but benign adaption to endurance sports. However, the changes could also mean that long-term training could result in overuse pathology with potentially deadly complications.
"Future studies aimed at defining the natural history of aortic dilation in this population with an emphasis on clinical outcomes ... will be required to resolve this fundamental uncertainty," the authors wrote. "In the absence of such data, clinical implications of our findings remain uncertain and will require individualized assessment."