Abstract
Background
Acoustic Radiation Force
Impulse (ARFI)-Imaging is an ultrasound-based elastography method enabling
quantitative measurement of tissue stiffness. The aim of the present study was
to evaluate sensitivity and specificity of ARFI-imaging for differentiation of
thyroid nodules and to compare it to the well evaluated qualitative real-time
elastography (RTE).
Methods
ARFI-imaging involves the
mechanical excitation of tissue using acoustic pulses to generate localized
displacements resulting in shear-wave propagation which is tracked using
correlation-based methods and recorded in m/s. Inclusion criteria were: nodules
≥5 mm, and cytological/histological assessment. All patients received
conventional ultrasound, real-time elastography (RTE) and ARFI-imaging.
Results
One-hundred-fifty-eight
nodules in 138 patients were available for analysis. One-hundred-thirty-seven
nodules were benign on cytology/histology, and twenty-one nodules were
malignant. The median velocity of ARFI-imaging in the healthy thyroid tissue,
as well as in benign and malignant thyroid nodules was 1.76 m/s, 1.90 m/s, and
2.69 m/s, respectively. While no significant difference in median velocity was
found between healthy thyroid tissue and benign thyroid nodules, a significant
difference was found between malignant thyroid nodules on the one hand and
healthy thyroid tissue (p = 0.0019) or benign thyroid nodules (p = 0.0039) on
the other hand. No significant difference of diagnostic accuracy for the
diagnosis of malignant thyroid nodules was found between RTE and ARFI-imaging
(0.74 vs. 0.69, p = 0.54). The combination of RTE with ARFI did not improve
diagnostic accuracy.
Conclusions
ARFI can be used as an
additional tool in the diagnostic work up of thyroid nodules with high negative
predictive value and comparable results to RTE.
Acoustic Radiation
Force Impulse (ARFI)-Imaging
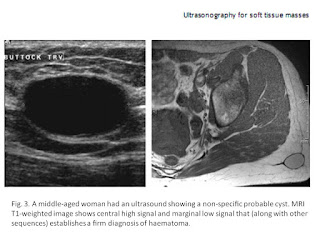
Velocities of ARFI measured in thyroid nodules and tissue
are shown in Table 3. In 5 patients no measurement in the healthy thyroid gland
was possible due to multinodular goiter. While no significant difference in
median velocity was found between healthy thyroid tissue and benign thyroid
nodules (p =0.068), a significant difference was found between healthy thyroid
tissue and malignant thyroid nodules (p =0.0019), as well as between benign and
malignant thyroid nodules (p = 0.0039), respectively.
The median success-rate of ARFI-measurement (number of valid
measurements divided by the number of all measurements performed) was 100% in
the healthy thyroid (mean: 99+/-2%, range: 91–100%), and 100% in thyroid nodules
(mean: 92+/-17%,range: 9–100%). The lower mean success-rate for nodules accounts
for the upper measurement limit of 8.4 m/s above which values were displayed as
‘‘x.xxm/s’’ and therefore counted as unsuccessful measurement.
AUROC for ARFI of the thyroid nodule for the diagnosis of
malignant thyroid nodules was 0.69 [95-CI: 0.53;0.85] (p = 0.0043). The optimal
cut-off with the highest sum of sensitivity and specificity (Youden cut-off)
for ARFI-measurement in thyroid nodules was 2.57 m/s (Table 2). AUROC for the
ratio of ARFI in the nodule and healthy
thyroid tissue for the diagnosis of malignant thyroid nodules was 0.71 [95-CI: 0.56;0.85] (p =
0.0025). The optimal cut-off (Youden cut-off) for ARFI-ratio was 1.57 m/s
(Table 2). No significant difference was found between AUROC of ARFI of the
nodule and ARFI-ratio (p.0.20). Details are shown in Table 2 and Figure 3.
Intra-observer variability expressed as the mean standard
deviation of 10 measurements at one location was 0.46 within all thyroid
nodules, and 0.21 within healthy thyroid tissue. It was higher in malignant
nodules with 0.94 as compared to benign nodules with 0.39.
Discussion
RTE has become a well
evaluated clinical tool enabling the determination of tissue elasticity using
ultrasound devices. RTE is a qualitative elastography method evaluating changes
in ultrasound pattern during strain and stress of direct or indirect tissue
compression. A recent meta-analysis reported a sensitivity and specificity for
RTE for the diagnosis of malignant thyroid nodules of 92%, and 90%,
respectively [12]. Methods to
quantify the colour coded images revealed by RTE were developed using strain
value and ratio and histograms with the aim of reducing intra- and
interobserver variability [27]–[29]. Nevertheless,
besides a lot of promising study results two recent studies have challenged the
usefulness of RTE in clinical practice by reporting no additional value as
compared to qualified B-mode ultrasound [13], [30].
Quantitative elastography was
well evaluated for the diagnosis of liver fibrosis with most studies evaluating
transient elastography (FibroScan, Echosens, Paris) [31]. Hereby, a
mechanical wave is send into the liver and the velocity of shear waves within
the liver is measured. However, it was only developed for measurement in liver
tissue. Recently, other quantitative elastography methods were developed, which
are integrated in conventional ultrasound systems and can be performed in all
solid organs [32], [33]. These
quantitative methods also send a mechanical or acoustic wave into the tissue
and measure the velocity of shear waves; the stiffer the tissue is, the faster
the shear waves propagate. Only one previous study with 146 nodules from 93
patients evaluated shear wave elastography with SuperSonic Imaging (Aixplorer, Aixen Provence ,
France
The combination of RTE with
ARFI-imaging improved specificity for the diagnosis of malignant thyroid
nodules from 72% (RTE alone) to 92% (combination of both), but reduced
sensitivity from 76% to 48%, respectively. Both methods revealed an excellent
negative predictive value for excluding malignant thyroid nodules with 95% for
RTE alone, and 93% for ARFI alone. The combination of both methods did not
further improve NPV.
A possible clinical algorithm
could be to use primarily one elastography method in combination with FNAB to
exclude malignancy of a thyroid nodule and perform follow-up examinations in
patients with benign FNAB and benign criteria on RTE or ARFI. However, both
methods might be useful in combination if FNAB reveals benign cytology, but one
elastography method shows criteria of malignancy. If then both methods (RTE and
ARFI) report values in the range of malignancy, than operation could be advised
despite the benign cytology. Nevertheless, of course B-mode ultrasound criteria
must be included in such an algorithm. Further larger studies are necessary to
find an optimal algorithm of B-mode ultrasound, qualitative and quantitative
elastography and FNAB to optimize the work up of thyroid nodules.
The present study has the
following limitations:
The reference standard was
cytology only in 94/158 (59.5%) nodules with benign cytology. However
ultrasound examination after 6 months did not show growth of nodule size as a
sign of benign lesions. Nevertheless, false-negative cytology may have existed.
Histology was the only excepted reference method for the diagnosis of malignant
thyroid nodules. The malignant nodules were predominantly papillary carcinoma
which might limit the diagnostic utility to this entity.
Cystic lesions without at
least 5×5 mm of solid parts of the nodules were excluded from the present
study, since ARFI –ROI measures 5×5 mm and cystic lesions produce artefacts on
RTE mimicking hard tissue. Therefore, the results of the present study cannot
draw any conclusion concerning the value of ARFI for predominantly cystic
lesions.
The guidelines for clinical
practice for the diagnosis and management of thyroid nodules of the American
Association of Clinical Endocrinologists (AACE), Associazione Medici
Endocrinologi (AME) and the European Thyroid Association recommend that
suspicious thyroid nodules smaller than 10 mm should be assessed by FNAB [5]. However, in the
present study, only 22 nodules with 5–10 mm in size were included, which was
too small to perform a subanalysis. A recent study demonstrated, that RTE can
be performed in thyroid nodules of 3–10 mm in size and is suitable for the
diagnosis of microcarcinoma of the thyroid gland [35]. Future studies
should evaluate the value of ARFI and the combination of ARFI with RTE in
thyroid nodules smaller than 10 mm.
The intra-observer
variability expressed as the mean standard deviation of 10 measurements at one
location was 0.46 within thyroid nodules, and 0.21 within healthy thyroid
tissue. Especially in malignant thyroid nodules it was as high as 0.94. A
reason might be that many measurements in malignant nodules resulted in “x.xx
m/s” if the value exceeded the upper detection limit of 8.4 m/s. In these cases
more than 10 measurement attempts were made to reach 10 numeric values. A
software optimization increasing the velocity detection at velocities exceeding
8.4 m/s are needed to overcome this limitation.
In summary, the present study
demonstrates comparable results for the novel quantitative Acoustic Radiation
Force Impulse-Imaging as for the well evaluated qualitative real-time
elastography for the differentiation of thyroid nodules. The combination of
both methods did not significantly improve the diagnostic accuracy for the
diagnosis of malignant thyroid nodules. Large multicenter studies are necessary
to develop application algorithms for qualitative and quantitative elastography
in clinical practice.