Tổng số lượt xem trang
Thứ Bảy, 21 tháng 8, 2021
Thứ Hai, 16 tháng 8, 2021
IVERMECTIN for PREVENTION and TREATMENT of COVID-19 INFECTION
Thông tin cơ bản: Đổi mục đích trị liệu của thuốc để chống lại vi rút SARS-CoV-2. Ivermectin vốn dùng diệt ký sinh trùng, với các đặc tính kháng vi-rút và chống viêm, hiện đã được thử nghiệm phòng chống vi rút SARS-CoV-2 trong nhiều thử nghiệm lâm sàng.
Các lĩnh vực không chắc chắn: Chúng tôi đã đánh giá hiệu quả điều trị của ivermectin trong việc giảm tỷ lệ tử vong, các tác dụng phụ trong trị liệu, ở những người có nguy cơ hoặc nguy cơ cao nhiễm COVID-19.
Nguồn dữ liệu:
Tìm dữ liệu để đánh giá cho đến ngày 25 tháng 4 năm 2021. Hai tác giả đã sàng lọc các nghiên cứu, trích xuất dữ liệu và đánh giá nguy cơ sai lệch. Các phân tích tổng hợp và tính chắc chắn của bằng chứng được đánh giá bằng cách sử dụng phương pháp GRADE và bổ sung trong các phân tích tuần tự thử nghiệm về tỷ lệ tử vong. Hai mươi bốn thử nghiệm ngẫu nhiên có đối chứng bao gồm 3406 người tham gia đã được xem xét.
Tiến bộ điều trị:
Phân tích gộp 15 thử nghiệm cho thấy ivermectin làm giảm nguy cơ tử vong so với không dùng ivermectin (tỷ lệ rủi ro trung bình 0,38, khoảng tin cậy 95% 0,19-0,73; n = 2438; I2 = 49%; bằng chứng chắc chắn trung bình). Kết quả này đã được xác nhận trong một phân tích tuần tự thử nghiệm sử dụng cùng một phương pháp DerSimonian-Laird làm cơ sở cho phân tích chưa điều chỉnh. Điều này với phân tích tuần tự thử nghiệm bằng phương pháp Biggerstaff-Tweedie cũng được xác nhận mạnh mẽ. Bằng chứng có độ chắc chắn thấp cho thấy dự phòng bằng ivermectin làm giảm nhiễm COVID-19 trung bình 86% (khoảng tin cậy 95% 79% -91%). Ảnh hưởng của tác dụng thứ phát cung cấp ít bằng chứng chắc chắn hơn. Ivermectin có thể không có lợi cho "nhu cầu thở máy" với bằng chứng có độ chắc chắn thấp, trong khi ước tính hiệu quả cho "cải thiện" và "suy giảm" rõ ràng được ưu tiên sử dụng ivermectin. Các tác dụng ngoại ý nghiêm trọng hiếm khi xảy ra trong các thử nghiệm điều trị và không có sự khác biệt được đánh giá với bằng chứng có độ chắc chắn thấp. Bằng chứng về các tác dụng phụ khác có độ chắc chắn rất thấp.
Kết luận: Ivermectin làm giảm tử vong do COVID-19 đáng kể với bằng chứng chắc chắn vừa phải [moderate-certainty evidence].
Sử dụng ivermectin sớm làm giảm số lượng ca nhiễm tiến triển thành bệnh nặng trong giai đoạn lâm sàng.
Tính an toàn và chi phí thấp cho thấy ivermectin có khả năng tác động đáng kể đến đại dịch SARS-CoV-2 trên toàn cầu.
Abstract
Background: Repurposed medicines may have a role against the SARS-CoV-2 virus. The antiparasitic ivermectin, with antiviral and anti-inflammatory properties, has now been tested in numerous clinical trials.
Areas of uncertainty: We assessed the efficacy of ivermectin treatment in reducing mortality, in secondary outcomes, and in chemoprophylaxis, among people with, or at high risk of, COVID-19 infection.
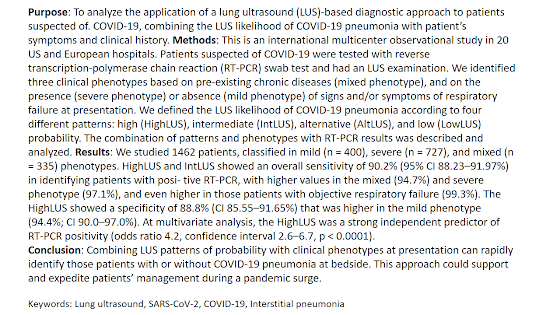
Data sources: We searched bibliographic databases up to April 25, 2021. Two review authors sifted for studies, extracted data, and assessed risk of bias. Meta-analyses were conducted and certainty of the evidence was assessed using the GRADE approach and additionally in trial sequential analyses for mortality. Twenty-four randomized controlled trials involving 3406 participants met review inclusion.
Therapeutic advances: Meta-analysis of 15 trials found that ivermectin reduced risk of death compared with no ivermectin (average risk ratio 0.38, 95% confidence interval 0.19-0.73; n = 2438; I2 = 49%; moderate-certainty evidence). This result was confirmed in a trial sequential analysis using the same DerSimonian-Laird method that underpinned the unadjusted analysis. This was also robust against a trial sequential analysis using the Biggerstaff-Tweedie method. Low-certainty evidence found that ivermectin prophylaxis reduced COVID-19 infection by an average 86% (95% confidence interval 79%-91%). Secondary outcomes provided less certain evidence. Low-certainty evidence suggested that there may be no benefit with ivermectin for "need for mechanical ventilation," whereas effect estimates for "improvement" and "deterioration" clearly favored ivermectin use. Severe adverse events were rare among treatment trials and evidence of no difference was assessed as low certainty. Evidence on other secondary outcomes was very low certainty.
Conclusions: Moderate-certainty evidence finds that large reductions in COVID-19 deaths are possible using ivermectin. Using ivermectin early in the clinical course may reduce numbers progressing to severe disease. The apparent safety and low cost suggest that ivermectin is likely to have a significant impact on the SARS-CoV-2 pandemic globally.
Copyright © 2021 The Author(s). Published by Wolters Kluwer Health, Inc.
Thứ Sáu, 13 tháng 8, 2021
TỰ SIÊU ÂM PHỔI BN COVID THEO DÕI TẠI NHÀ
In conclusion, we present a new mechanism for monitoring patients with COVID-19 in the home, using a novel teleguidance system for LUS that can be used by the patient (or by EMS).
Integrating LUS into home management could decrease the need for patients to be transported to a hospital or imaging center, avoiding unnecessary disease transmission through patient movement. Further work to investigate a larger implementation into common telehealth platforms and the ease of use by lay people and their caregivers is warranted.
Impact of the coronavirus disease 2019 pandemic on irritable bowel syndrome
Abstract
Background and Aim: Gastrointestinal manifestations of the coronavirus disease 2019 (COVID-19) pandemic may mimic irritable bowel syndrome (IBS), and social distancing measures may affect IBS patients negatively. We aimed to study the impact of COVID-19 on respondents with self-reported IBS.
Methods: We conducted an anonymized survey from May to June 2020 in 33 countries. Knowledge, attitudes, and practices on personal hygiene and social distancing as well as psychological impact of COVID-19 were assessed. Statistical analysis was performed to determine differences in well-being and compliance to social distancing measures between respondents with and without self-reported IBS. Factors associated with improvement or worsening of IBS symptoms were evaluated.
Results: Out of 2704 respondents, 2024 (74.9%) did not have IBS, 305 (11.3%) had self-reported IBS, and 374 (13.8%) did not know what IBS was. Self-reported IBS respondents reported significantly worse emotional, social, and psychological well-being compared with non-IBS respondents and were less compliant to social distancing measures (28.2% vs 35.3%, P = 0.029); 61.6% reported no change, 26.6% reported improvement, and 11.8% reported worsening IBS symptoms. Higher proportion of respondents with no change in IBS symptoms were willing to practice social distancing indefinitely versus those who deteriorated (74.9% vs 51.4%, P = 0.016). In multivariate analysis, willingness to continue social distancing for another 2–3 weeks (vs longer period) was significantly associated with higher odds of worsening IBS.
Conclusion: Our study showed that self-reported IBS respondents had worse well-being and compliance to social distancing measures than non-IBS respondents. Future research will focus on occupational stress and dietary changes during COVID-19 that may influence IBS.
Thứ Năm, 12 tháng 8, 2021
Acute Hepatitis Caused by Asymptomatic COVID-19 Infection
A 30-years old woman was admitted at the emergency department for mild fever, anosmia and dysgeusia from 10 days. She denied cough, sore throat, shortness of breath, diarrhea, nausea, vomiting, or abdominal pain. Her parents and an uncle were diagnosed positive for COVID-19 infection in the previous three days. She did not have any chronic disease and she was not taking any drug at the time of admission. A nasopharyngeal swab was promptly done and RT-PCR resulted positive for COVID-19 infection. Chest X-ray did not show findings compatible with interstitial pneumonia; arterial oxygen saturation was 99% on room air. On presentation, her temperature was 36 °C. There were no cutaneous manifestations, her lung examination was normal, and there was no jaundice, right upper quadrant tenderness, hepatomegaly, or splenomegaly. Laboratory results were as follows: AST 1531 IU/L (normal value < 35), ALT 893 IU/L (normal < 36), serum bilirubin 1.02 mg/dL (normal < 1.2), alkaline phosphatase 106 IU/L (normal 33–98), INR 1, gammaglutamiltransferase 1276 IU/L (normal < 40), white blood cells 4070 cells/mm3 (normal 4000–10,000), platelets 152,000 cells/mm3 (normal 150,000–450,000). She denied recent intake of reliever drugs as paracetamol or antibiotics in the previous weeks.
The abdominal ultrasound did not show significant abnormalities of liver, gallbladder, kidneys, spleen, pancreas and abdominal vessels.
The following serological tests were performed and all were negative: hepatitis A, B, C, E, Cytomegalovirus, EpsteinBarr and respiratory viral panel. Blood cultures for bacteria and fungi, and the screening for autoimmune diseases were also negative. She was then treated with infusion of saline solution 0.9% (1500 cc/daily) with progressive reduction of liver abnormalities. In particular, after 3 days laboratory results were: AST 111 IU/L, ALT 89 IU/L, alkaline phosphatase 97 IU/L and gammaglutamiltransferase 246 IU/L. No respiratory symptom occurred during follow-up and the patient was discharged after 5 days of hospitalization, in good clinical condition and asymptomatic from both hepatic and respiratory point of view. At our knowledge, this is the first report of COVID-19 infection presenting as acute hepatitis in absence of respiratory symptoms. Our patient had very mild symptoms related to COVID-19 infection and was only tested due to her familiar cluster. Other possible causes of liver abnormalities were ruled out, therefore it seems likely that acute hepatitis was directly caused by COVID19. Recently, Wander et al.8 described a non-icteric, acute hepatitis in an HIV-infected woman, but their patient developed overt respiratory symptoms in the hours immediately following diagnosis and also had other possible causes of liver tests abnormalities such as the use of concomitant drugs and a fair number of co-morbidities. Mild-to moderate liver test abnormalities are becoming a frequent finding in subjects admitted to hospital for COVID-19 infection. Patients with known risk factors for COVID-19 infection presenting with acute hepatitis should be rapidly isolated and tested. In our patient, the abnormalities in liver function tests quickly normalized, in absence of specific therapy. The real meaning of liver tests transient alterations has yet to be determined in COVID19 infected subjects. With the future evolution of the pandemic, prospective observations could provide further information on this specific clinical issue.
References
[1]. Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020;395:507–13.
[2]. Rothe C, Schunk M, Sothmann P, Bretzel G, Froeschl G, Wallrauch C, et al. Transmission of SARS-CoV-2 infection from an asymptomatic contact in Germany. N Engl J Med 2020;382:970–1.
[3]. Holshue ML, DeBolt C, Lindquist S, Lofy KH, Wiesman J, Bruce H, et al. First case of 2019 novel coronavirus in the United States. N Engl J Med 2020;382:929–36.
[4]. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497–506.
[5]. Phipps MM, Barraza LH, LaSota ED, Sobieszczyk ME, Pereira MR, Zheng EX, et al. Acute Liver Injury in COVID-19: prevalence and association with clinical outcomes in a large US cohort. Hepatology 2020 Online ahead of print. doi:10.1002/hep.31404.
[6]. Wang Y, Liu S, Liu H, Li W, Lin F, Jiang L, et al. SARS-CoV-2 infection of the liver directly contributes to hepatic impairment in patients with COVID-19. J Hepatol 2020 May 11;S0168-8278(20)30294-4. doi:10.1016/j.jhep.2020.05.002.
[7]. Kunutsor SK, Laukkanen JA. Hepatic manifestations and complications of COVID-19: a systematic review and metanalysis. J Infect 2020;81(3):e72–4. doi:10.1016/j.jinf.2020.06.043.
[8]. Wander P, Epstein M, Bernstein D. COVID-19 presenting as acute hepatitis. Am
Chủ Nhật, 8 tháng 8, 2021
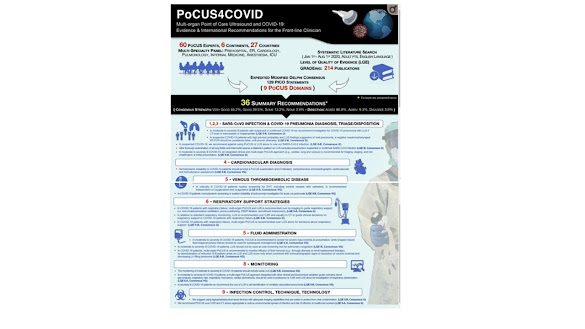
Poc U S and COVID-19
Thứ Sáu, 6 tháng 8, 2021
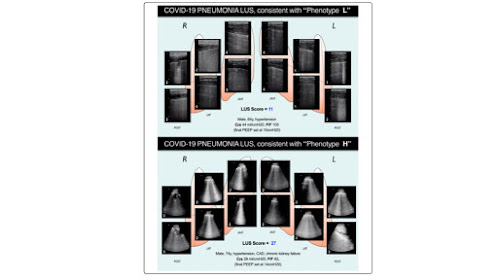
SIÊU ÂM PHỔI [LUS] TRONG MÙA DỊCH COVID-19
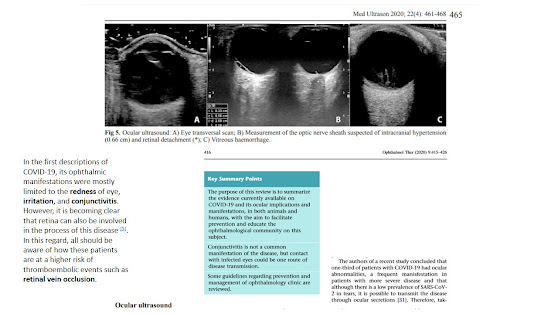
Prof. Wang: I also want to point out that looking at the other organs – the kidneys, the liver and the heart – is very important. COVID-19, because of low oxygen, will affect those organs. Echocardiography is an important part of critical care ultrasound because the heart is the center of oxygen transport. So, timely and routine echocardiography examination for the patient is very important. For the kidney, we look at it with imaging, with color and with Doppler. Even in traditional sepsis, the secondary injury is also important, and we need to pay more attention to it.
Dr. Jalil: When I’m putting a probe on a patient, it’s usually after I’ve talked to them or am trying to figure out what’s going on. I’m trying to add ultrasound to my physical exam. On the ventilator you can look at the compliance of the lungs, you can look at trends. Another way is looking at bilateral B-lines. It can tell you which direction the lungs are going and if the treatment is helping or not.
Dr. Villén: I look at three particular things: B-lines, subpleural consolidations and the thickness of the pleural line. In my opinion, the most sensitive places to put the probe and find something is the posterior below the arm and the axillar point. If you find just subpleural consolidation posterior, probably these are related to mild disease. Keep in mind this is a quite new virus for us. We are learning every day.
How are you using ultrasound to scan the lungs of COVID19 patients?
Prof. Wang: Lung ultrasound is very important in monitoring the lung deterioration in COVID-19 patients, especially for critical patients. ICU doctors have learned that critical care ultrasonography can be used to manage and monitor the lungs of critical COVID patients. We have two methods of monitoring these patients. ICU doctors are using lung ultrasound at the very beginning [when patients are admitted] and when patients are critical, like respiratory and circulatory issues.
Dr. Villén: The findings in lung ultrasound of patients with COVID-19 or any other viral pneumonia is based on three findings: 1) The subpleural consolidations, which is an area of small pneumonia in the border of the lung. Generally, it's triangular with a base with the pleura and the vortex pointed towards the lung; 2) The B-lines--so, an appearance which indicates no edema--in this case there is no fluid. It’s not a matter of fluid, but a matter of initial inflammation which cells fiber; 3) A thickened pleura, which is kind of the same of the subpleural consolidation, but it's more related to an area not a small spot.
In my opinion, the most sensitive places to put the probe and find something is in the posterial, below the arm and the axillar point – they are the most sensitive and not common when performing a lung examination. Most subpleural consolidations are posterior or between lateral and posterior and these are not normal points we normally use for lung examination. And the anterior chest is only affected in severe patients in my experience. If you move only into the anterior lateral, you will not find anything if the patient has coronavirus. So, you will go posterior for more superior and apical more axillar and this are not as tender of points of examinations.
How does point-of-care ultrasound compare with other imaging options in the context of COVID-19?
Prof. Wang: More and more doctors are recognizing the role of ultrasound for monitoring of COVID-19 patients. Point of care ultrasound is portable and can be right at the beside making it convenient and repeatable.
Dr. Jalil: I don’t think this replaces any modalities that I use today. The whole point of being able to do point of care ultrasound it to extend your physical exam. It gives quick information. If I walk into a patient’s room, I can very quickly get images and figure out if this is a pneumothorax, the heart or something different. In the emergent situation, ultrasound is easier to squeeze into a room than an X-ray machine. Handheld ultrasound takes it one step further – just having it in my pocket is convenient.
Dr. Villén: Right now, we cannot afford to send the patient to a CT scan and wait two hours until it is clean again. We need something quick, fast, and reliable that can be made at the bedside, if possible, so I am using ultrasound. With ultrasound, first you must control the environment, cover the machine or at least the probes, dress yourself in protective gear. After performing the examination, you have to go out of the room, take your clothes off and clean the machine for every patient. This process takes 10 to 15 minutes.
What advice would you share with other healthcare providers using ultrasound to help treat and monitor COVID-19 patients?
Prof. Wang: The key principle is do everything early. Detection, monitoring, testing, treatment, isolation, and IPC - infection prevention and control. The earlier you diagnose, the better the outcome.
Dr. Jalil: We can minimize daily x-rays and prevent some of the spread by thinking of trends, for example, what the lungs look like. A lot of times in the ICU you’re trying to keep their volume to the lowest. One or two way to achieve this – on the ventilator you can look at the compliance of the lungs or you can look at the trends. Another way is looking at bilateral B-lines. It can also tell you which direction the lungs are going and if the treatment is helping or not.
Dr. Villén: Go more posterior than you think. Don’t rely on the basic views of lung ultrasound.
This was already described for acute respiratory distress syndrome (ARDS) which is what COVID is. We are seeing ARDS in early stages at least at the emergency department and in different states of the progression of the disease. That’s why it’s quite new for us, because we know how ARDS behaves in the ICU, but not in the emergency department. It’s a matter of time evolving of the disease.
Thứ Ba, 27 tháng 7, 2021
Mô tuyến vú trên siêu âm liên quan đến nguy cơ ung thư vú
Từ AuntMinnie.com
Ngày 21 tháng 7 năm 2021 - Mô tuyến có liên quan đến nguy cơ ung thư vú trong tương lai ở phụ nữ có mô vú đặc theo một nghiên cứu về phụ nữ ở Hàn Quốc được công bố ngày 19 tháng 7 trên tạp chí Radiology .
Các nhà nghiên cứu dẫn đầu bởi đồng tác giả Tiến sĩ Su Hyun Lee, Tiến sĩ và Tiến sĩ Han-Suk Ryu, từ Đại học Quốc gia Seoul, Hàn Quốc cho biết với những phát hiện này, thành phần mô tuyến trong siêu âm vú nên được xem xét để phân tầng nguy cơ trong quá trình sàng lọc.
Tăng mật độ vú khi chụp nhũ ảnh, được xác định bởi số lượng mô sợi liên quan đến mô mỡ trên hình ảnh, là một yếu tố nguy cơ ung thư vú. Nó cản trở việc phát hiện ung thư vú vì che khuất và làm khó phân biệt giữa mô tuyến và mô xơ.
Nhóm nghiên cứu muốn tìm ra mối liên quan giữa thành phần mô tuyến khi siêu âm tầm soát và nguy cơ ung thư vú ở phụ nữ có mô vú đặc Nhóm cũng muốn tìm ra mối liên hệ giữa thành phần mô tuyến và sự tiến hóa của tiểu thùy.
Xem xét dữ liệu thu thập từ 8.483 phụ nữ từ năm 2012 đến năm 2015 không có tiền sử ung thư vú và độ tuổi trung bình là 49 tuổi. Những người được siêu âm vú và có mô vú đặc với kết quả âm tính trước đó từ chụp nhũ ảnh. Có 137 ca trong số này phát triển ung thư vú với thời gian theo dõi trung bình là 5,3 năm.
Nhóm nghiên cứu phát hiện ra rằng thành phần mô tuyến vừa phải hoặc nhiều có liên quan đến tăng nguy cơ ung thư theo độ tuổi và mật độ vú. Tuy nhiên, điều ngược lại cũng được xác định là đúng với diễn tiến phát triển của tiểu thùy.
Cần xác nhận thêm về thành phần mô tuyến trong quá trình siêu âm sàng lọc vú. Điều này có thể hữu ích trong việc phân tầng nguy cơ ung thư vú và nhu cầu kiểm tra bổ sung ở phụ nữ có mô vú đặc.
Họ cũng kêu gọi các nghiên cứu trong tương lai so sánh thành phần và sự phát triển của tiểu thùy tại cùng một vị trí trong vú.
CT and US provide chance for fatty liver disease screening
By AuntMinnie.com staff writers
May 25, 2021 -- Abdominal CT and ultrasound can be useful tools for opportunistic screening for hepatic steatosis, or fatty liver disease, according to a study published May 24 in the Journal of the American College of Radiology.
Hepatic steatosis is a common incidental finding on abdominal imaging, a group led by Dr. Rubal Penna of Virginia Mason Medical Center in Seattle noted. But it's not always taken seriously, despite the fact that it is associated with liver disease, cirrhosis, and diabetes.
In the new study, Penna's group explored whether adding a standardized note regarding incidentally identified hepatic steatosis to a patient's radiology report would not only help referring clinicians follow up but also identify significant disease.
The study included 1,256 patients who underwent either CT or ultrasound and whose reports included a note about the presence of hepatic steatosis between April 2016 and September 2017. The researchers assessed whether any follow-up clinical action had been taken in response, tracking patient demographics, type of referring provider, and urgency of exam results.
Follow-up was more likely for patients whose exams had been ordered by primary care providers, whose exam results weren't urgent, and who had undergone ultrasound. Follow-up of the study cohort found fatty liver disease in 70%, nonalcoholic steatohepatitis in 6%, and alcoholic hepatitis in 17%.
"Opportunistic screening for incidental hepatic steatosis on abdominal CT and ultrasound is feasible, with substantial yield for patients with clinically important entities including nonalcoholic fatty liver disease and nonalcoholic steatohepatitis," the team concluded.